Proper Skin Assessment

Welcome to this video on skin assessment! The skin is the largest organ of the body and has many areas involved in its assessment. In this video, I’ll be focusing on a general assessment of the skin as well as how to implement measures to maintain skin integrity and prevent skin breakdown.
Gathering Data
Diseases of the skin may be local, or they may be caused by an underlying systemic problem. In order to perform a complete and accurate assessment, the nurse needs to collect data about current symptoms, the patient’s past and family history, and health and lifestyle practices.
When looking at current symptoms, ask the patient:
- About skin problems such as rashes, dryness, oiliness, bruising, open sores, itchiness, etc.
- Any birthmarks or moles?
- Any change in the ability to feel pain, pressure, touch, or temperature?
- Any numbness or tingling?
- Trouble controlling body odor?
- Any body piercings or tattoos?
Guideline for collecting the needed information about symptoms:
Character – Describe the sign or symptom
Onset – When did it begin?
Location – Where is it?
Duration – How long does it last? Does it recur?
Severity – How bad is it? Does it bother you?
Pattern – What makes it better or worse?
Associated factors / How it affects the patient?What other symptoms occur with it? How does it affect you?
When assessing past health history, ask the patient:
- To describe any previous skin problems and any treatment or surgery that was done.
- Any allergic skin reactions?
- Any recent fever, N/V, or respiratory problems?
- (For female patients) Are you pregnant? Are menstrual cycles regular?
- Any history of smoking or drinking alcohol?
- Any history of anxiety, depression, or other psychiatric problems?
When looking at the family history, ask the patient:
- Has anyone in your family had a recent illness, allergy, rash, or other skin problem?
- Anyone in your family had skin cancer?
- Any family history of keloid scars?
Some skin conditions tend to be hereditary or contagious, so it is beneficial to know what the patient has been exposed to and what runs in their family.
Lifestyle and health practices play a big role in the assessment of skin. Ask the patient:
- Do you sunbathe or tan?
- Are you regularly exposed to chemicals that may harm the skin, such as paint, bleach, cleaning products, petroleum, insect repellant, etc.?
- Do you spend a long time sitting or lying in one position?
- Any exposure to extreme temperatures?
- What do you use daily on your skin, such as soaps, lotions, oils, cosmetics, and type of razor?
- What do you eat and drink in a typical day?
- Do skin problems limit any of your normal activities or prevent you from enjoying relationships?
- Describe the stress in your life.
- Do you perform a monthly skin self-examination?
The physical assessment of the skin involves inspection and palpation and may reveal local or systemic problems in the patient.
Inspection involves looking at the following:
General skin color – abnormal findings would include pallor, cyanosis, or jaundice
Color variations – look for rashes or erythema
Skin integrity – carefully check pressure point areas
Lesions – note the color, shape, and size
When palpating the skin, it is important to note:
Texture – it should be smooth and even.
Thickness – very thin skin may indicate steroid therapy or arterial insufficiency.
Moisture – increased moisture is felt with fever and
hyperthyroidism, decreased moisture occurs with dehydration or hypothyroidism.
Temperature – cool skin may accompany arterial disease, cold skin is felt in shock or hypotension, and very warm skin is felt with fever or hyperthyroidism.
Turgor – refers to the skin’s elasticity and should pinch easily, then immediately return to its original position.
Edema – the skin should rebound and not remain indented when pressure is released.
Skin Ulcers
A very common skin problem you will encounter as a nurse is the pressure ulcer, also known as a bedsore. Pressure ulcers are localized injuries to the skin and underlying tissue that nearly always develop in areas where there are bones right under the skin. This includes the heels, ankles, tailbone, hips, elbows, shoulder blades, ears, and back of the head.
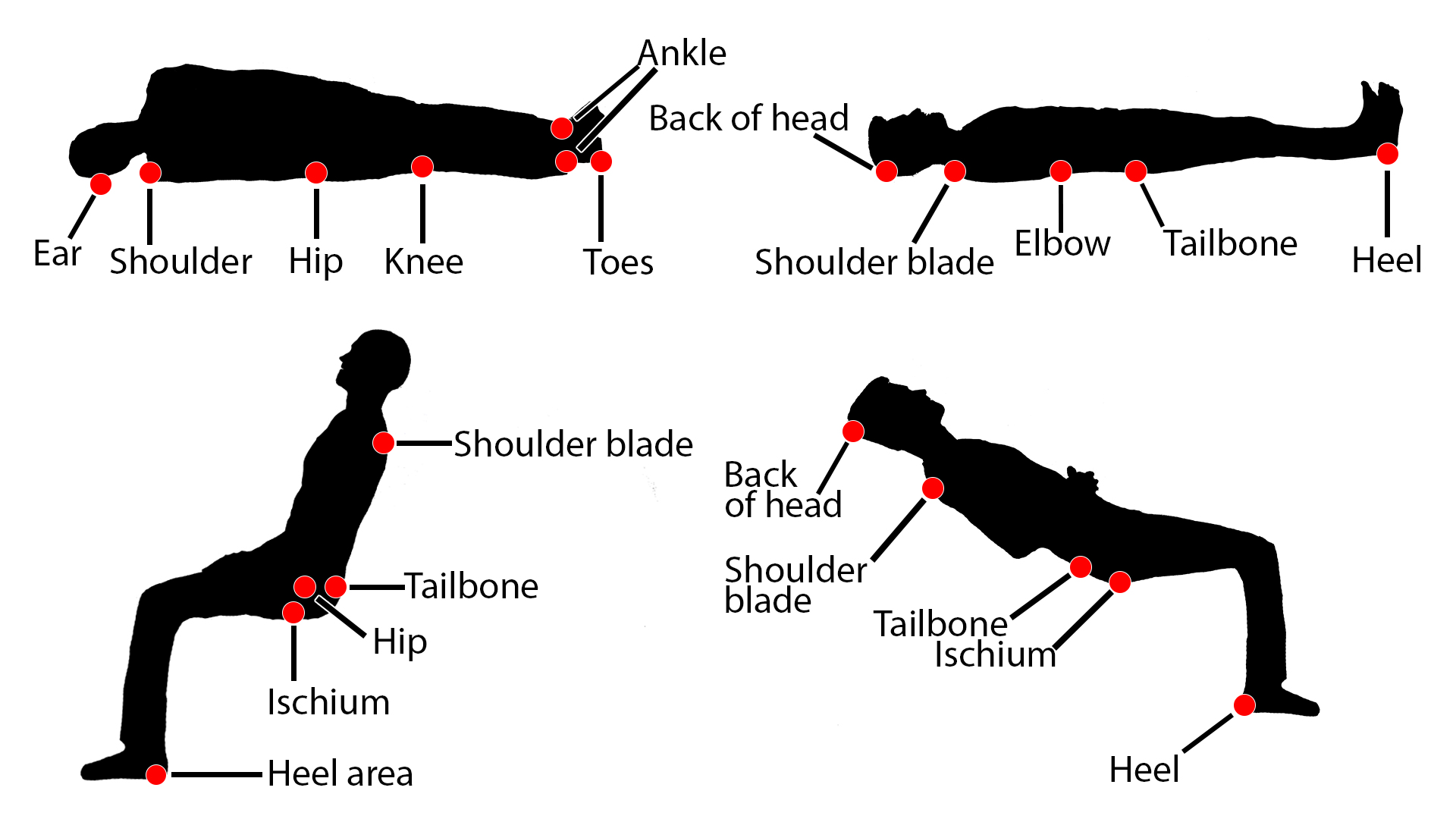
If body weight is continually putting pressure in places where a person is sitting or lying for a long time, not enough blood can get through to provide oxygen and nutrients. The skin becomes thinner, and over time it gradually dies, creating an open wound. Risk factors for skin breakdown leading to pressure ulcers include poor circulation, poor hygiene, infrequent position changes, infection, dermatitis, or traumatic wounds. Pressure ulcers can lead to sepsis and even death, and they are much easier to prevent than to treat.
As a nurse, it is extremely important to assess the patient’s skin adequately and carry out preventative measures. For an initial assessment of the potential to develop a pressure ulcer, use the Braden Scale. This assessment tool measures:
Sensory perception – the ability to respond meaningfully to
pressure-related discomfort.
Moisture – the degree to which skin is exposed to moisture.
Activity – the degree of physical activity.
Mobility – the ability to change and control body position.
Nutrition – the usual food intake pattern.
Friction and shear
The nurses’ responsibility for assessing and preventing pressure ulcers includes the following:
- Inspect the skin at least daily, or more often if high risk, using a risk assessment tool, such as the Braden Scale.
- Bathe with mild soap and warm water, limiting friction.
- Use incontinence skin cleansing methods as needed.
- Avoid shear and friction by using careful positioning, turning, and transferring techniques.
- Be aware of patient’s dietary needs, especially if protein-deficient. Refer to a dietitian.
If the patient is bed or chair-bound:
- Reposition or teach self-reposition every 15 minutes (chair) or 2 hours (bed).
- Use a chair cushion or pressure mattress.
- Position with pillows or wedges to maintain body alignment and avoid bony prominence contact with surfaces.
- Use lifting devices if available to reduce shear.
- For the bed-bound, avoid elevating the head of bed except for short periods.
If a patient has to sit or lie down without moving for a long time—even if just for a few days—it is important to reduce pressure on the parts of the body that are most at risk.
Remember, document everything you do, because in the medical-legal world, if you didn’t document it, you didn’t do it.
Thank you for watching this video tutorial on skin assessment!
