Pediatric Advanced Life Support

Hi, and welcome to this video on the American Heart Association’s pediatric advanced life support, or PALS. We will discuss the recommended algorithms for cardiac arrest and symptomatic bradycardia in this video.
According to the American Heart Association data from 2008 through 2017, approximately 15,000 in-hospital pediatric cardiac arrest events occur annually. Some of the most common causes of cardiac arrest include congenital heart defects, sports injuries (such as from impact with a ball in the chest), and exposure to drugs (such as cocaine and inhalants).
Advanced pediatric life support is carried out by medical personnel, such as paramedics, doctors, and nurses, with access to the appropriate training, medications, and resuscitation equipment.
Under the pediatric cardiac arrest algorithm, if a child enters into cardiac arrest, the first step is to initiate CPR within 10 seconds of arrest, using a rate of 15 compressions to 2 ventilations. The compressions should be provided at a depth of about one-third of the anteroposterior chest diameter and at a rate of 100 to 120 compressions per minute. In some situations of pediatric cardiac arrest, other individuals (such as bystanders or non-licensed personnel) may have already started CPR, but as a medical professional that is trained in providing advanced interventions, you should relieve them.
Next, bag-mask ventilation should be provided as soon as possible, with oxygen provided at a concentration of 100%. If an advanced airway is established, administer oxygen through the airway and give one breath every 2 to 3 seconds or 20 to 30 breaths per minute, while compressions are provided continuously.
Non-Shockable and Shockable Rhythms
Next, attach the monitor/defibrillator if it’s not already in place and conduct a rhythm check to determine if the rhythm is shockable or non-shockable. Compressions must be held while the defibrillator is analyzing the rhythm.
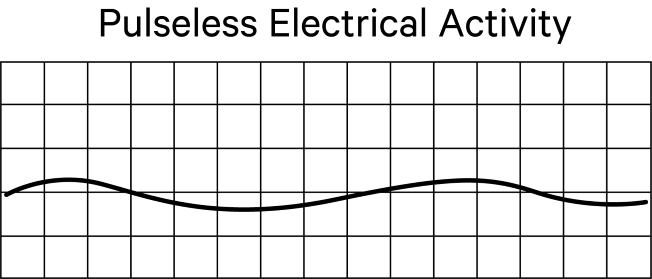
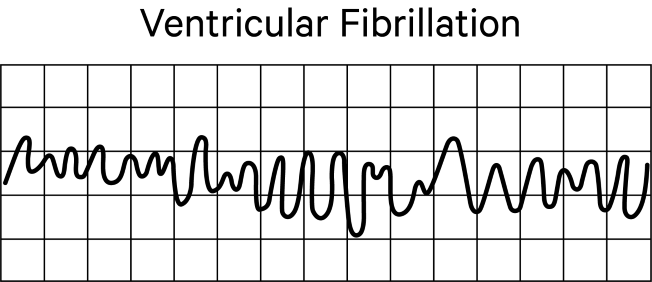
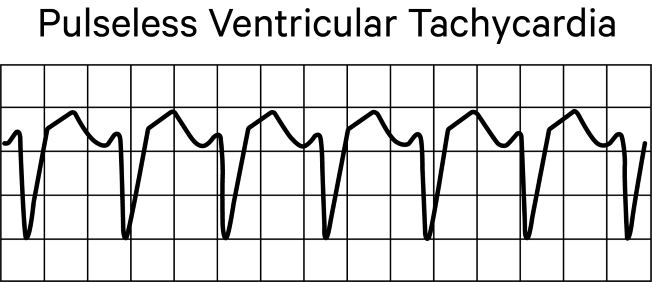
Non-shockable rhythms include asystole and pulseless electrical activity. Shockable rhythms include ventricular fibrillation and pulseless ventricular tachycardia.
Let’s look first at interventions for non-shockable rhythms.
On an electrocardiogram or monitor, asystole is characterized by a flat line, which indicates that both electrical and mechanical activities of the heart have stopped. We sometimes say that a patient has “flatlined.”
With pulseless electrical activity, the tracing will show electrical activity but the mechanical functioning of the heart is not adequate to produce a palpable pulse. This is also referred to as electromechanical dissociation. For this reason, it is critical that pulse checks are being performed in conjunction with an analysis of the heart rhythm.
Once a non-shockable rhythm has been identified, it’s critical to administer epinephrine as soon as possible, and repeat administration every 3 to 5 minutes as needed. If you are carrying out bag-mask ventilation, you may consider an advanced airway and capnography.
Continue to check the rhythm and pulse every two minutes, as the rhythm may convert to normal sinus or may convert to a shockable rhythm. In both cases, interventions would change based on the rhythm. An AED will prompt these rhythm checks every 2 minutes. If the rhythm remains non-shockable, continue with the CPR in between rhythm checks.
Here are some things to remember about pediatric life support for non-shockable rhythms:
- First, change compressors every 2 minutes or sooner if the compressor becomes fatigued.
- Interruptions to CPR should last no more than 10 seconds for pulse and rhythm checks every 2 minutes.
- If an advanced airway is in place with capnography, which assesses carbon dioxide levels, a low or decreasing patient end-tidal carbon dioxide level can indicate a problem with CPR. The normal value for end-tidal CO2 is 35 to 40 millimeters of mercury. Less than 10 millimeters of mercury indicates ineffective compressions.
- Intravenous access is preferable to intraosseous access, but speed is important so avoid repeatedly trying for IV access.
- The pediatric dose for epinephrine is 0.1 milliliters per kilogram of the 0.1 milligrams per milliliter concentration intravenously or intraosseously every 3 to 5 minutes to maximum dose of 1 mg. If intravenous or intraosseous access is not available, you may give an endotracheal dose of epinephrine at 0.1 milliliter per kilogram of the 1 milligram per milliliter concentration.
- An advanced airway may include an endotracheal tube (cuffed preferred over uncuffed) or supraglottic advanced airway. Use waveform capnography or capnometry to confirm and monitor endotracheal tube placement.
- With an advanced airway in place, provide 1 breath every 2 to 3 seconds without interrupting compressions.
Now, let’s look at shockable rhythms, which include ventricular fibrillation and pulseless ventricular tachycardia.
With ventricular fibrillation, the ventricles quiver instead of adequately contracting. This quivering does not supply sufficient cardiac output to perfuse the brain and other vital organs, and is very dangerous. The electrocardiogram or monitor tracing is irregular with unformed QRS complexes and an absence of clear P waves.
With pulseless ventricular tachycardia, ventricular contractions are very rapid but ineffective because the ventricles are unable to fill adequately, so cardiac output falls. The tracing is characterized by a wide QRS complex and a rate greater than 180 per minute.
Remember that with a non-shockable rhythm, the first thing you do is administer epinephrine because a shock would be ineffective. However, with a shockable rhythm, it’s essential that you administer a shock as soon as the AED or defibrillator is available.
After the shock, immediately resume CPR for 2 minutes and establish intravenous or intraosseous access. Check the rhythm again after these 2 minutes, and if it remains shockable, give a second shock, and then immediately resume CPR and begin to administer epinephrine every 3 to 5 minutes. An advanced airway and capnography should also be considered at this point.
Check the rhythm again and, if a shockable rhythm persists, give a third shock before resuming CPR. At this point, you may administer amiodarone or lidocaine and treat reversible causes if the shockable rhythm persists.
Reversible causes of cardiac arrest to be considered include the 5 Hs and 5 Ts:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypo or hyperkalemia
- Hypothermia
- Tension pneumothorax
- Cardiac tamponade
- Toxins
- Pulmonary thrombosis AND
- Coronary thrombosis
Critical Considerations
Here are some important points to remember about life support for ventricular fibrillation and pulseless ventricular tachycardia:
- First, for defibrillation, use 2 joules per kilogram for the first shock, 4 joules per kilogram for the second shock, and greater than or equal to 4 joules per kilogram to a maximum of 10 joules per kilogram for subsequent shocks. Use adult AED pads if pediatric attenuated pads are not available. If the pads touch one another when both are placed on the chest, then place one pad on the anterior chest and the other on the patient’s back. Anterior-posterior placement is usually required for infants and children up to 8 years of age.
- Next, the dosage for epinephrine is the same as for non-shockable rhythms at 0.1 milliliter per kilogram of the 0.1 milligram per milliliter concentration intravenously or intraosseously every 3 to 5 minutes to maximum dose of 1 mg. If intravenous or intraosseous access is not available, you may give an endotracheal dose of epinephrine at 0.1 milliliter per kilogram of the 1 milligram per milliliter concentration.
- If using amiodarone, give 5 milligrams per kilogram intravenously or intraosseously during cardiac arrest and you can repeat this up to 3 total doses for refractory ventricular fibrillation or pulseless ventricular tachycardia.
- If using lidocaine instead of amiodarone, give 1 milligram per kilogram as a single loading dose.
- Continue CPR with an advanced airway as you would for non-shockable rhythms.
- Last, remember to take no more than 10 seconds for pulse and rhythm checks every 2 minutes, usually while also changing compressors.
Let’s take a minute to review some additional considerations for pediatric cardiac arrests:
- First, respiratory arrest with a pulse is more common in infants and young children than in adults, so be aware of that. In these cases, only rescue breathing is provided with continuous pulse checks.
- If arterial blood pressure monitoring is in place, use the diastolic blood pressure to assess the quality of the CPR. Aim for greater than or equal to 25 millimeters of mercury for infants and greater than or equal to 30 millimeters of mercury for children.
- Avoid the routine use of cricoid pressure with endotracheal tube intubation.
- Use cuffed endotracheal tubes, but choose the correct size and position, and maintain pressure at greater than 20 to 25 centimeters of water.
- Last, for bag-mask ventilation, use 450 milliliters for infants and small children, and 1,000 milliliters for larger children and adolescents.
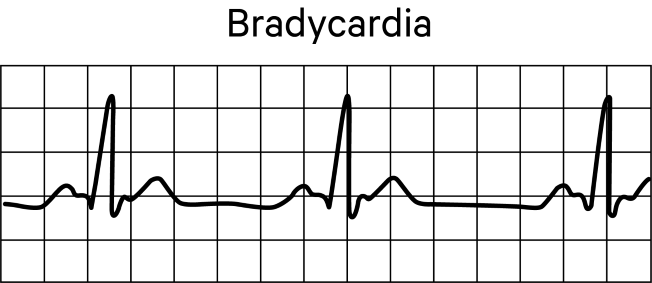
Next, let’s take a look at the American Heart Association’s algorithm for pediatric bradycardia. Typically, the heart rate of infants and young children is faster than that of adults, so a pulse rate below 60 beats per minute in this demographic may indicate distress and should trigger an assessment.
According to the pediatric advanced life support algorithm for bradycardia, first consider whether there is cardiopulmonary compromise. Signs of cardiopulmonary compromise include:
- Acutely altered mental status
- Signs of shock AND
- Hypotension
If there are no signs of cardiopulmonary compromise, then
- Monitor and support the patient’s airway, breathing, and circulation, as needed.
- If oxygen saturation is borderline low, consider administering oxygen via nasal cannula or face mask.
- Obtain a 12-lead electrocardiogram to monitor the heart rhythm AND
- Consider treating any possible underlying causes of the bradycardia, such as hypothermia, hypoxia, and medications.
If, however, the bradycardia persists and there are signs of cardiopulmonary compromise, then
- Closely monitor the airway, and use an alternative or advanced airway if necessary
- Provide oxygen at a concentration of 100% using positive pressure ventilation if necessary
- Connect the patient to a cardiac monitor to assess the patient’s heart rhythm, pulse, blood pressure, and oximetry.
If the child’s heart rate falls below 60 beats per minute despite these interventions, start CPR and reassess the rhythm in two minutes to determine if the bradycardia persists. If the heart rate has increased adequately, continue to provide support and monitor.
Note that bradycardia is diagnosed based on age. Bradycardia is considered in an infant with a heart rate of less than 100, less than 80 in young children, less than 70 in school children, and less than 60 in adolescents. So, generally speaking, if the heart rate falls below 60 in an infant or child, perfusion is likely inadequate.
Therefore, if the bradycardia persists and the pulse remains below 60 beats per minute, interventions are critical. You must:
- Continue CPR
- Establish intravenous or intraosseous access and administer epinephrine.
- If there is increased vagal tone or the ECG shows a primary AV block, administer atropine.
- Consider transthoracic or transvenous pacing.
- Identify and treat underlying causes.
- Continue to check the patient’s pulse every 2 minutes.
- If there is ever NO pulse, immediately transition to the cardiac arrest algorithm.
Here are some things to remember about treating bradycardia in an infant or child:
- First, administer epinephrine at 0.1 milliliter per kilogram of the 0.1 milligram per milliliter concentration every 3 to 5 minutes.
- If an endotracheal tube is in place and intravenous or intraosseous access is not available, administer endotracheal epinephrine at 0.1 milliliter per kilogram of 1 milligram per milliliter concentration.
- For intravenous or intraosseous atropine, give 0.02 milligrams per kilogram with a minimum dose of 0.1 milligram and maximum dose of 0.5 milligrams. This may be repeated for one additional administration.
- Administer CPR and initiate an advanced airway in the same manner used for shockable and non-shockable rhythms.
In conclusion, whether the child has experienced a cardiac arrest with a non-shockable or shockable rhythm or bradycardia with cardiopulmonary compromise, time is the essential element. Every minute that treatment is delayed increases the risk of neurologic compromise and death.
That’s all for this review. Thanks for watching, and happy studying!
