Patellar Fractures

Hi, and welcome to this review of patellar fractures! In this video, we’ll quickly go over the anatomy of the patellar area and then discuss how patellar fractures happen and how different types of patellar fractures are managed. Let’s get started!
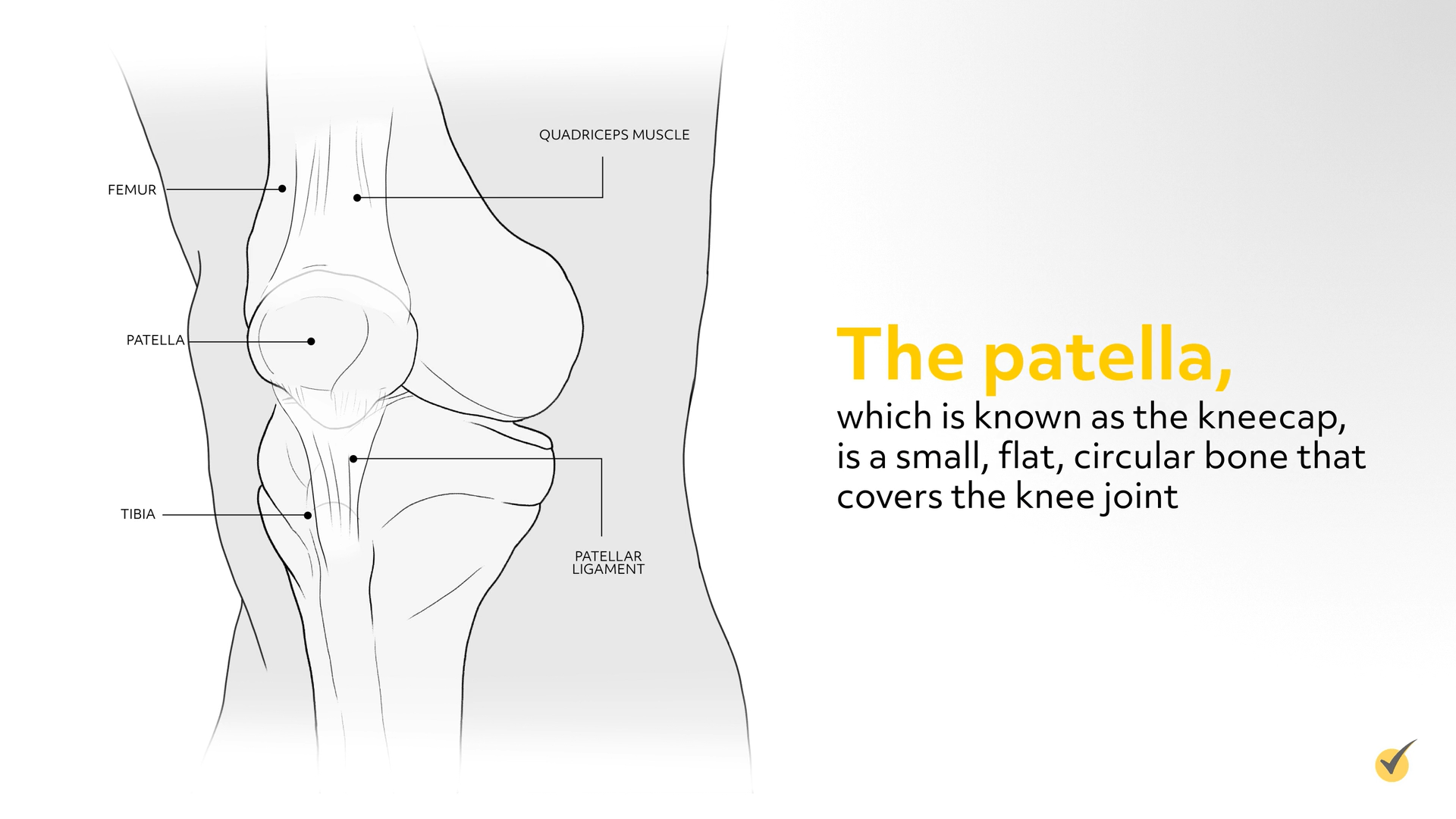
So, firstly, let’s remind ourselves of what the patella actually is. The patella, which is known as the kneecap, is a small, flat, circular bone that covers the knee joint. There are two main functions of the patella. The first is to give the quadriceps femoris muscles a mechanical advantage in extending the knee. The second is to protect the knee joint.
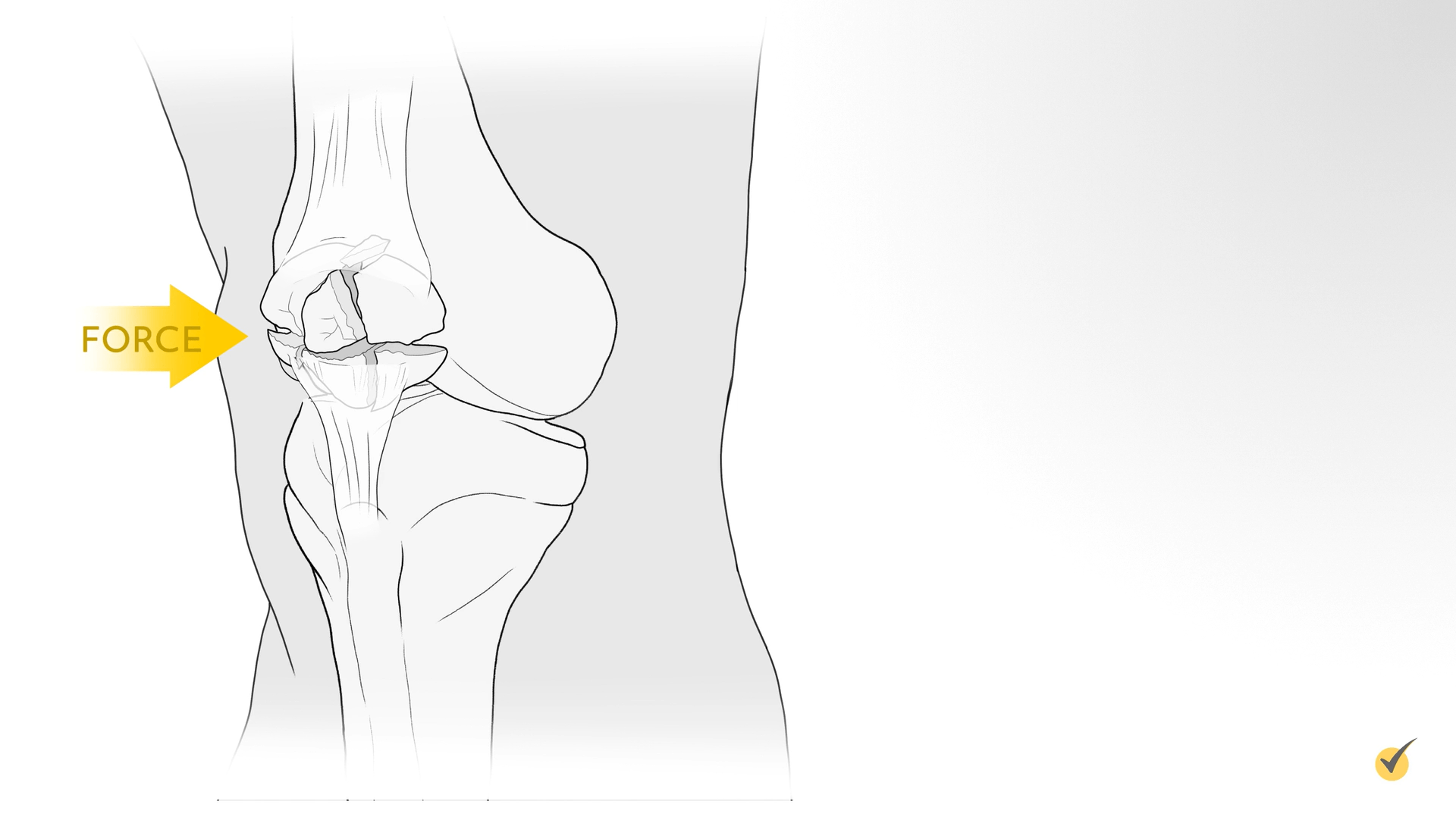
There are several different ways someone might cause trauma to their patella. They might have been involved in a car accident where the patella is forced forward against the dashboard. Perhaps they fell directly on the knee or some moving object hit their knee.
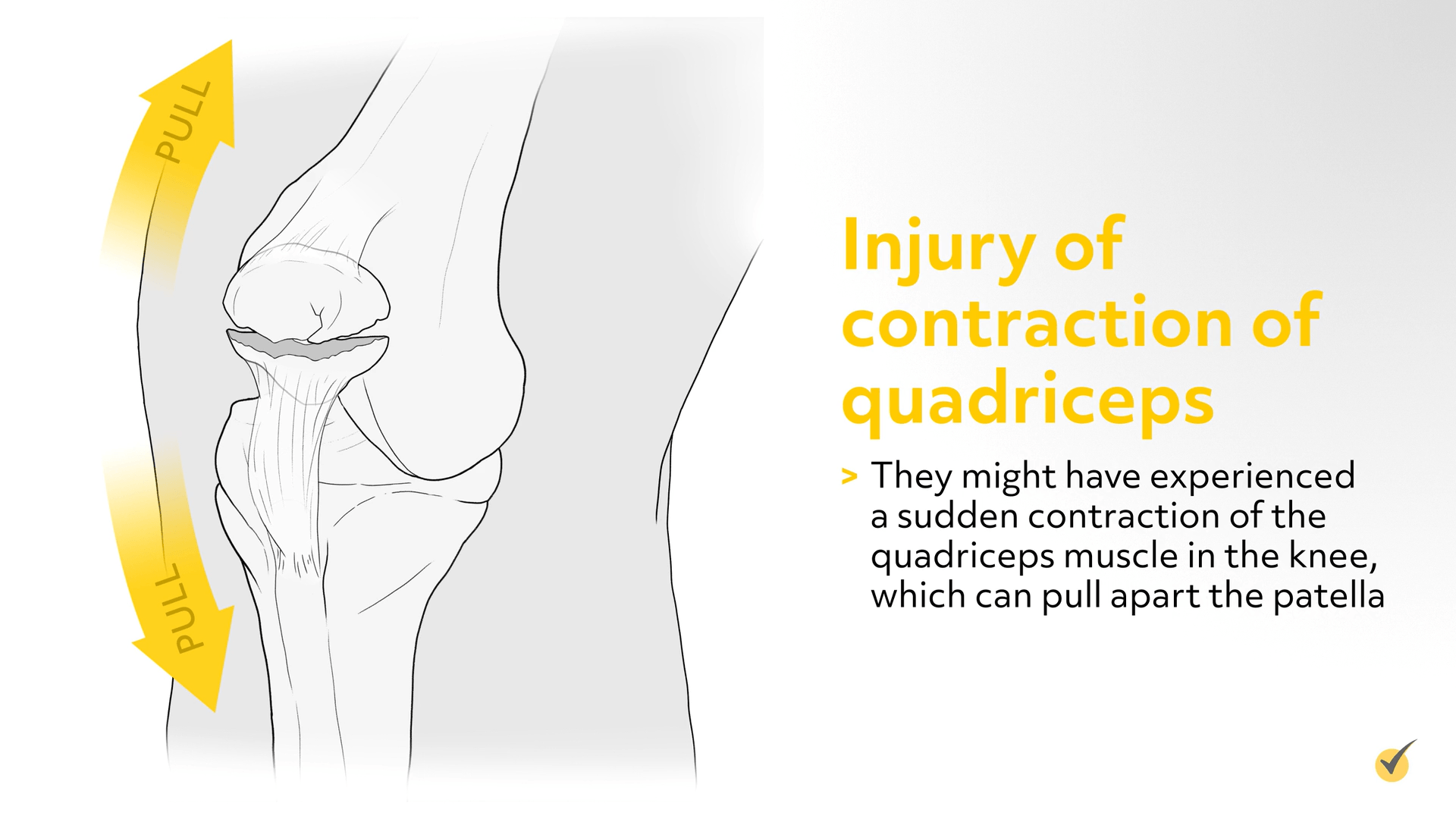
Or, they might have experienced a sudden contraction of the quadriceps muscle in the knee, which can pull apart the patella.
Depending on the trauma that occurred, there are a few different types of patellar fractures that may result. The first one we’re going to look at is the “nondisplaced fracture.”
A nondisplaced or stable fracture is a break in the patella bone, but the bone continues to be aligned (or stable) and the pieces of the bone generally remain in contact with each other. If there is a space of separation in the bone, it is only a millimeter or two apart.
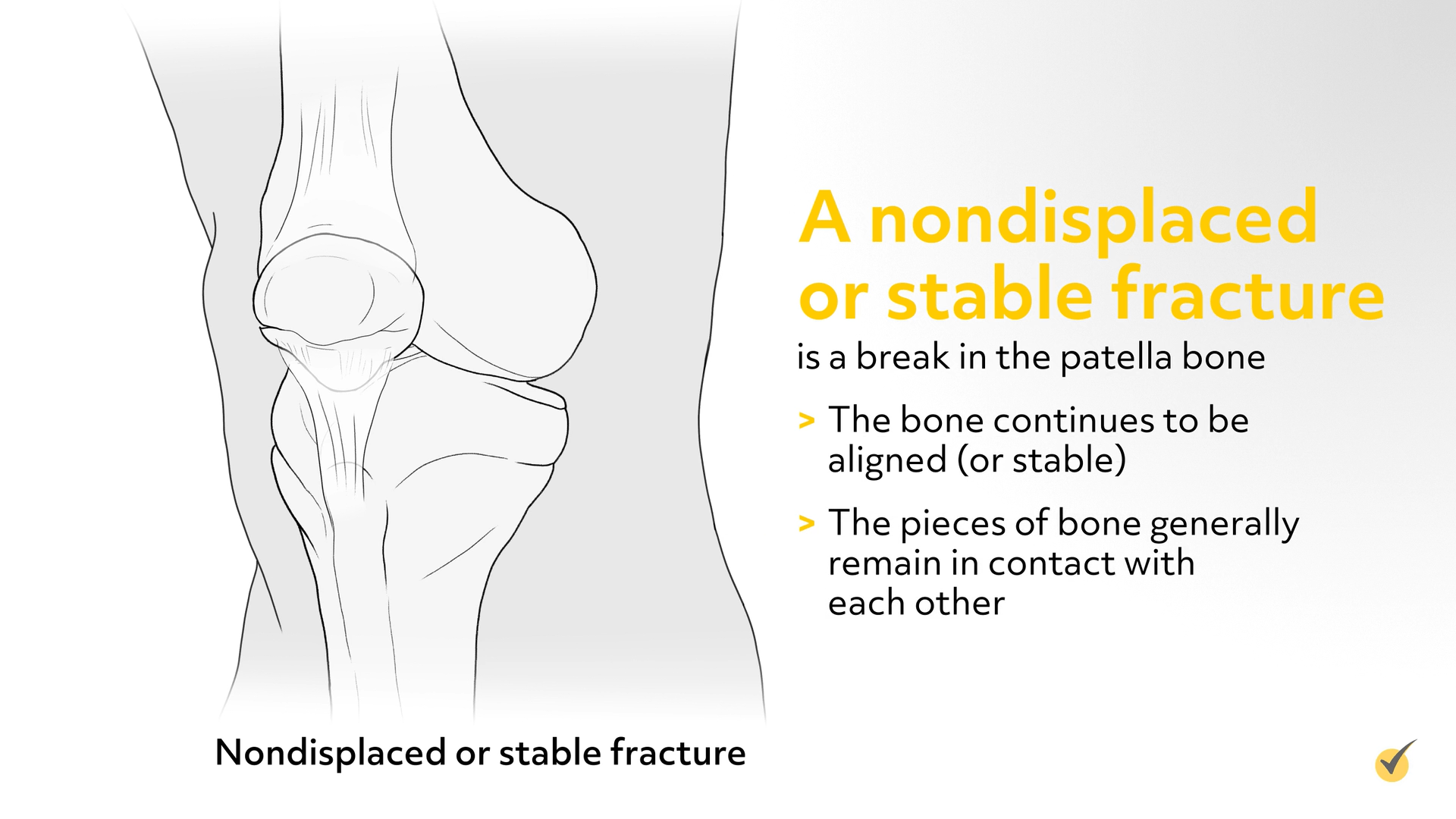
If the fracture is nondisplaced, the orthopedic doctor can align the bone with closed reduction or with a long leg cast or other immobilizer with the knee in full extension. Depending on the extent of the fracture, the patient might be able to bear weight on it immediately or have to keep weight off the leg for up to 6-8 weeks. X-rays of the area will diagnose the fracture and usually guide treatment.
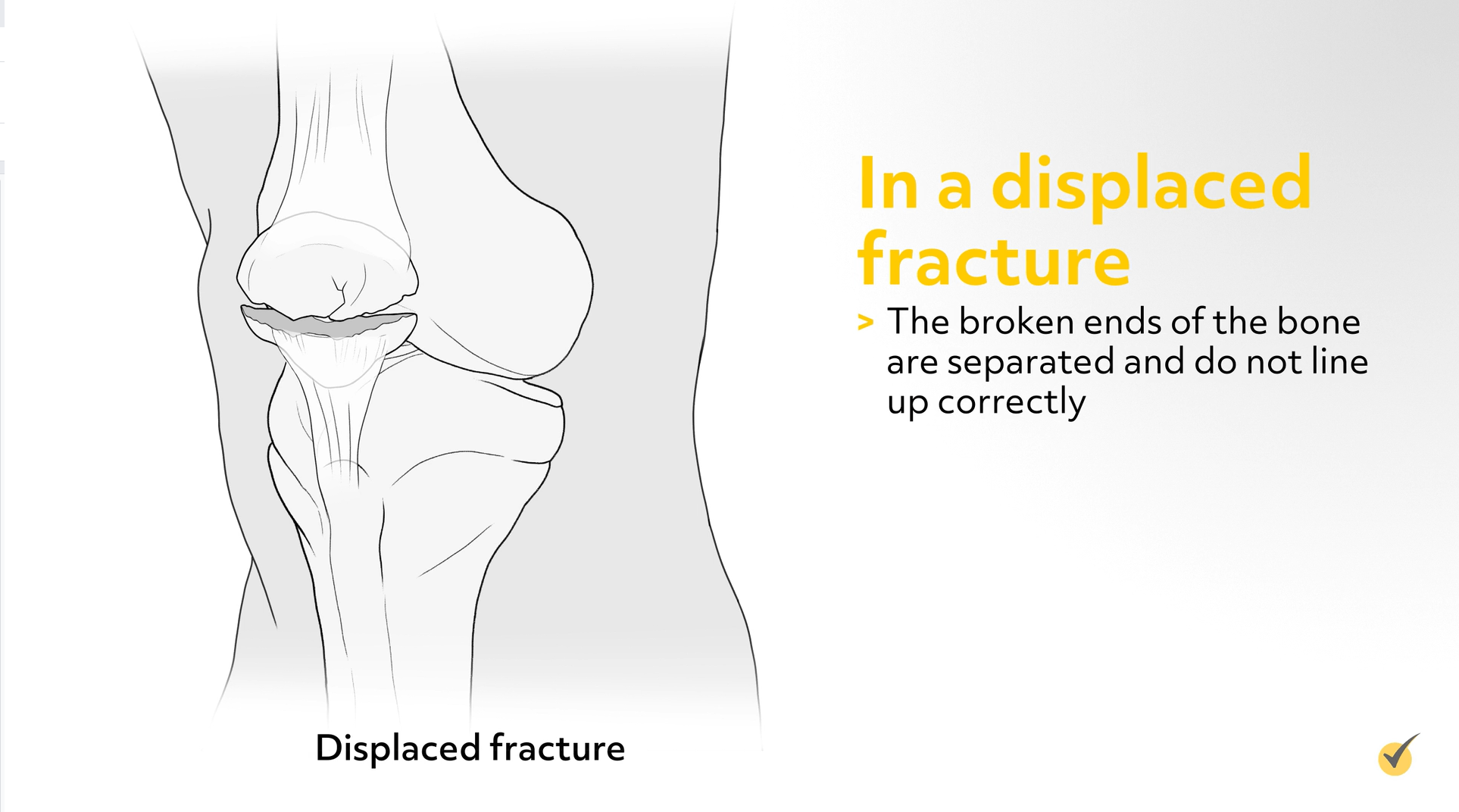
In a displaced fracture, the broken ends of the bone are separated and do not line up correctly. This separation could be vertical or transverse. The normally smooth joint surface may also be disrupted. This type of fracture often requires open-reduction internal fixation (ORIF) and continuous passive motion to manage properly.
If ORIF is being used to manage the fracture, the orthopedic surgeons will make an incision in the affected area, reduce the bone if necessary, realign it, and internally fix it in place with wires, pins, or screws.
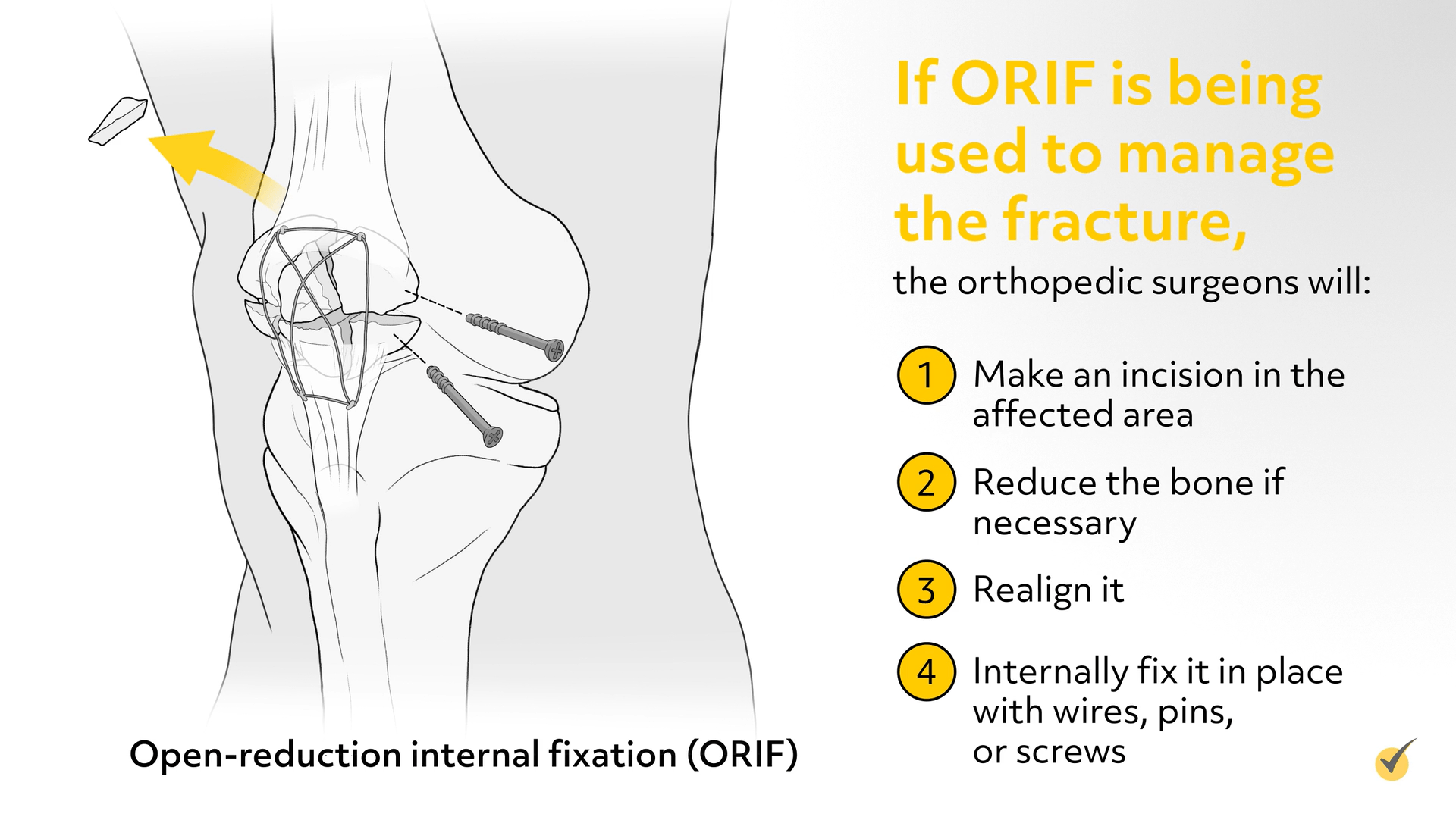
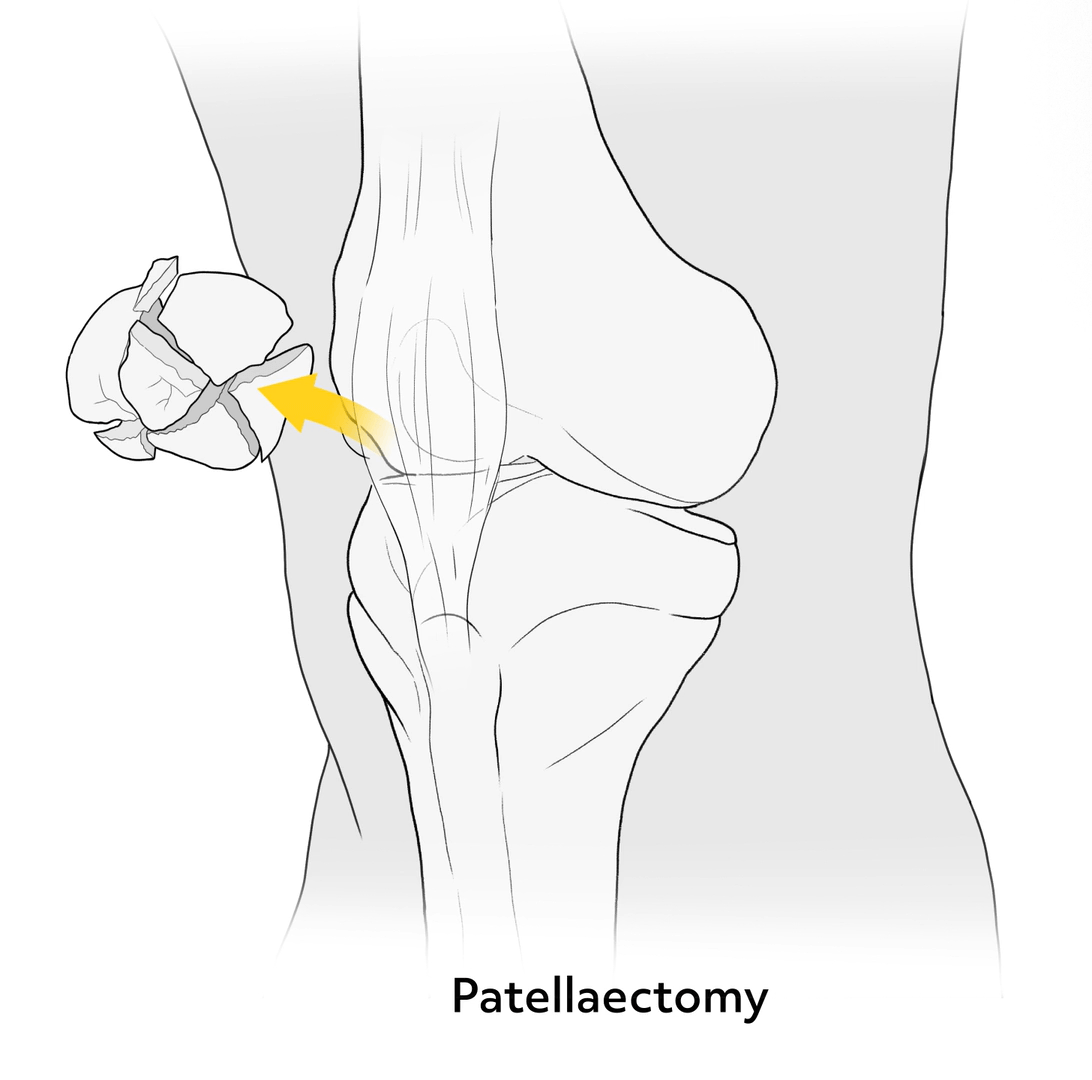
The purpose and goal of this procedure is for the patient to be able to regain or maintain use of the knee joint for bending, leg straightening, and walking. In rare cases, if the patella cannot be repaired this way, the patient’s patella may be removed, which would affect normal movement.
Appropriate physical therapy interventions for displaced and nondisplaced fractures are partial or weight-bearing, making sure the fracture is not stressed. For a displaced fracture, eventual active-assisted range of motion exercises may be required.
The final type of patellar fracture we’ll be looking at is the comminuted patella fracture. With this type of fracture, there are many breaks in the bone. The “shattered” bone can appear aligned (nondisplaced) or not aligned (displaced).
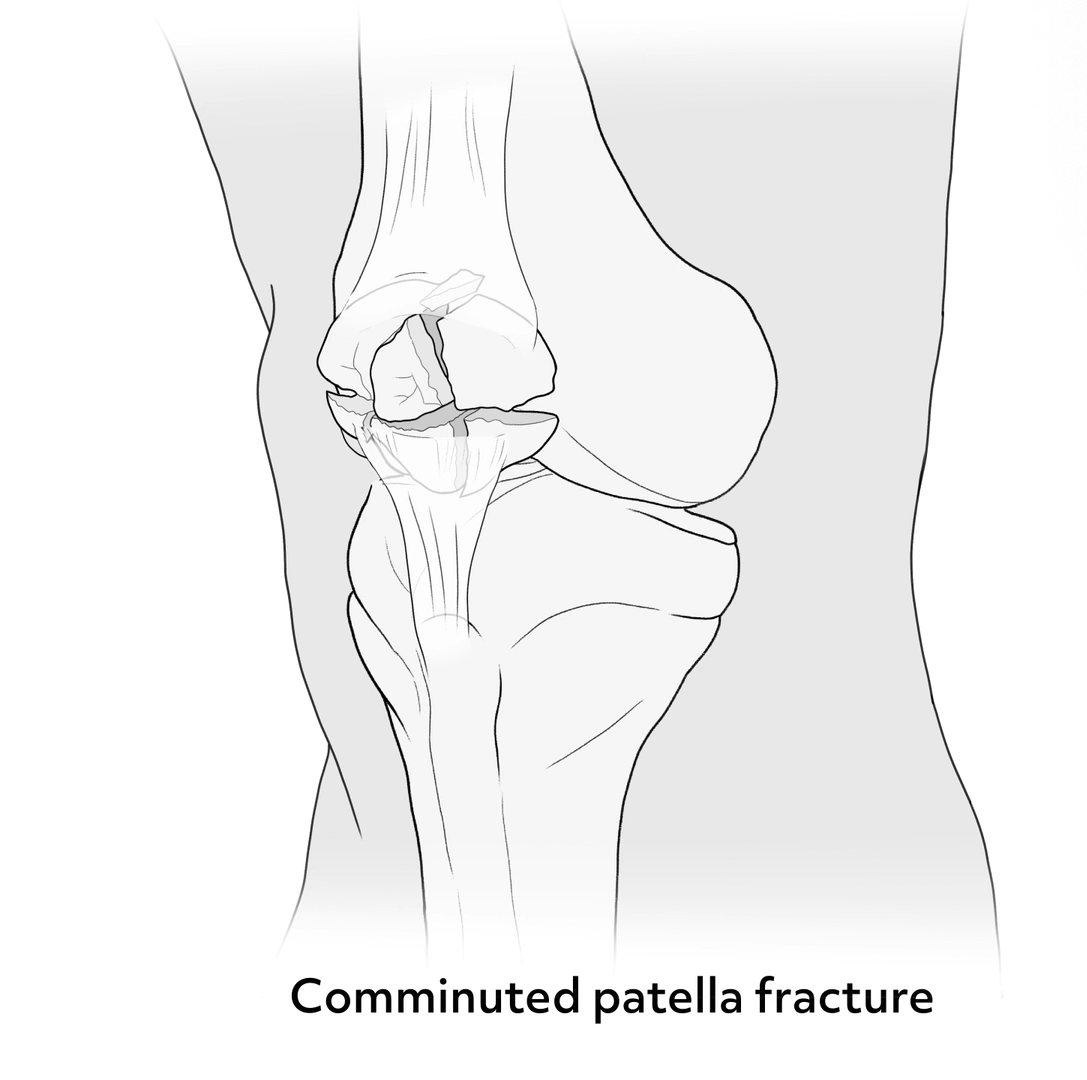
Comminuted patellar fractures are managed with ORIF, a partial or total patellectomy with quadriceps tendon repair, or immobilization using a long leg cast or brace or a posterior splint with the knee in full extension or minimal flexion.
If the bone fragments are too small to be fixed back into place, the orthopedic surgeon will remove them. He or she will then attach the loose patellar tendon back to the remaining patellar bone. If the kneecap is broken in many pieces at its center and the pieces are separated, the orthopedic surgeon may use a combination of wires and screws to fix it. Removing small portions of the kneecap that cannot be reconstructed may also have positive results. Complete removal of the kneecap is a last resort in treating a comminuted fracture.
Recovery from a patella fracture requires a few main points to be addressed. First and foremost is pain management. This can be done initially with ice and elevation and over-the-counter pain medications if the pain is not severe. For more severe pain, the doctor will prescribe something to manage the pain, which can last from days to weeks. Next to consider is rehabilitation. Because the leg may be immobilized for a period of time to allow healing, the patient will want to work on regaining motion, relieving stiffness, and getting back to moving through physical therapy, which should also include strengthening exercises around the knee joint. Regaining strength and mobility will take time and depend on the severity of the injury.
Alright, before we go, let’s go over a couple of review questions to see what you remember.
1. Which type of fracture is being described here?
“A break in the patella bone, but the bone continues to be stable”
- Comminuted
- Displaced
- Nondisplaced
- Open
The correct answer is C! A nondisplaced or stable fracture is a break in the patella bone, but the bone continues to be aligned (or stable) and the pieces of the bone generally remain in contact with each other.
2. True or false: Open reduction internal fixation is the most common way to manage nondisplaced patellar fractures.
The correct answer is False! Open reduction internal fixation is not used to manage nondisplaced fractures but is often used to manage displaced and comminuted fractures.
That’s all for this review! Thanks for watching, and happy studying!
