
Hi, and welcome to this video about multiple organ dysfunction syndrome!
We’re going to look at an overview of the disease, the signs and symptoms, diagnosis, and management.
Let’s get started!
Multiple organ dysfunction syndrome (MODS) refers to an acutely ill patient that has progressive organ dysfunction, in which homeostasis cannot be maintained without intervention. It is a process rather than a single event, and it is at the severe end of illness severity of both infectious and noninfectious conditions.
It can be classified as primary or secondary:
- Primary MODS is the result of a definite insult to an organ, in which organ dysfunction occurs early and can be directly attributed to the insult itself.
- Secondary MODS refers to organ failure that occurs as a result of the patient’s response to an illness, often sepsis, rather than a direct insult to the organ.
Our focus today will be on secondary MODS, caused by sepsis.
Sepsis
Sepsis is a clinical syndrome in which a severe infection becomes complicated and is characterized by systemic inflammation and widespread tissue injury. The clinical process usually begins with infection, which can lead to sepsis and then organ dysfunction.
Symptoms of sepsis are typically nonspecific and include fever and chills, along with more specific symptoms of malaise, fatigue, confusion, or anxiety. Since there is a continuum of severity from sepsis to septic shock to MODS, the specific symptoms exhibited depend on where the patient falls on the continuum. Look for signs of a localized infection.
Assessment of the patient’s overall condition usually reveals an acutely ill, toxic appearance in patients with serious infections. Tachypnea is common, as well as tachycardia with an increased pulse pressure. In the early stages of sepsis, cardiac output is well maintained or even increased, but as sepsis progresses, stroke volume and cardiac output fall. Patients begin to have poor distal perfusion, including cool extremities, cool skin, and delayed capillary refill.
Localized infections often present with the following physical signs:
- Central nervous system infection – exhibits profound depression in mental status.
- Head and neck infections – cause inflamed or swollen tympanic membranes, sinus tenderness, stridor, pharyngeal exudates, or cervical lymphadenopathy.
- Chest and pulmonary infections – cause localized rales or lung consolidation.
- Cardiac infections – cause a regurgitant valvular murmur.
- GI infections – exhibit abdominal tenderness, rectal tenderness, or swelling.
- Pelvic and GU infections – cause pelvic or adnexal tenderness, and/or renal tenderness.
- Bone and soft tissue infections – exhibit redness, edema, and tenderness.
- Skin infections – often show up as petechiae and purpura.
SOFA
A scoring system is utilized to assess the severity of organ dysfunction in patients who are critically ill from sepsis. SOFA (Sequential Organ Failure Assessment) uses simple measurements of major organ function to calculate a severity score, with the highest score most predictive of mortality.
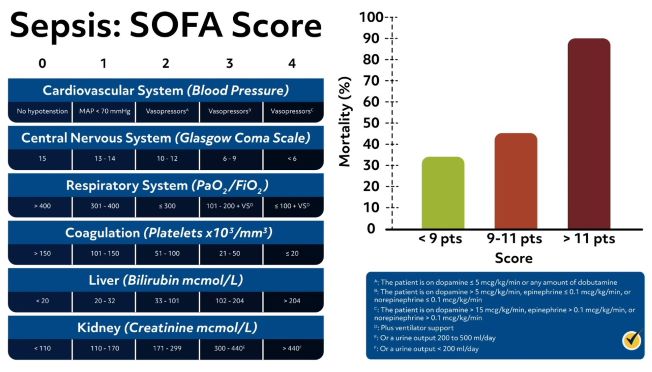
The SOFA severity score is based on the following organ function measurements:
- Respiratory system – the ratio of PaO2 to FiO2
- Cardiovascular system – the amount of vasoactive medicine required to prevent hypotension
- Hepatic system – the bilirubin level
- Coagulation system – the platelet concentration
- Neurologic system – the Glasgow coma score
- Renal system – the serum creatinine or urine output
The SOFA score is used as a tool to facilitate the identification of patients at risk of dying from sepsis.
Diagnosis
Diagnosis of MODS involves laboratory tests to identify sepsis in order to assess the general hematologic and metabolic condition of the patient.
- A CBC with differential is necessary to evaluate oxygen delivery in shock, and with persistent sepsis, the platelet count will fall. The White Blood Cell count and differential can predict the existence of a bacterial infection.
- A complete metabolic panel (CMP) will assess serum electrolytes, as well as renal and hepatic function.
- Serum lactate assesses tissue hypoperfusion – elevated levels indicate that significant tissue hypoperfusion exists, signaling a worse degree of shock and higher mortality.
- PT and aPTT will assess coagulation status and evidence of coagulopathy would require additional tests to detect disseminated intravascular coagulation (DIC).
- Blood cultures can be used to diagnose intravascular infections and infections of indwelling intravascular devices.
- A urinalysis and urine culture should be done since urinary infection is a common source of sepsis, especially in the elderly.
- Secretions or tissue of Gram stain and culture should be obtained from sites of potential infection.
Various imaging methods are also used to diagnose focal infections and evaluate complications of sepsis and septic shock.
- A chest X-ray can diagnose pneumonia infiltrates. X-ray can also help identify a deep soft tissue infection.
- Ultrasound is used when a biliary tract infection is suspected as the source of sepsis.
- Computed tomography (CT) is utilized when assessing for an intra-abdominal abscess or a retroperitoneal source of infection. A CT scan of the head should be obtained when there is increased intracranial pressure, suspected focal mass lesions, or before lumbar puncture when meningitis is suspected.
Forms of MODS
There are two forms of multiple organ dysfunction syndrome. In both, the development of acute lung injury (ALI) or ARDS is the earliest manifestation.
More Common
In the more common form of MODS, the lungs are the predominant, and often the only organ system affected until very late in the disease. Patients often present with a primary pulmonary disorder, such as pneumonia, contusion, aspiration, near drowning, hemorrhage, exacerbation of COPD, or pulmonary embolism.
When the lung disease progresses, encephalopathy or mild coagulopathy may occur, persisting for 2-3 weeks. At this point, the patient either begins to recover or progresses to a sudden dysfunction in another organ system. Once another major organ dysfunction occurs, these patients frequently do not survive.
Less Common
The second form of MODS presents with the causative source in organs other than the lungs – most commonly intra-abdominal sepsis, pancreatitis, extensive blood loss, or vascular catastrophes. ARDS still develops early and dysfunction in other organ systems also develops much sooner than in the first form of MODS.
For several weeks, patients remain in a pattern of compensated dysfunction, at which time they either recover or deteriorate further and die.
Treatment
When we look at treatment for multiple organ dysfunction syndrome, it is not so much a syndrome to be treated, but a complication to be prevented. Treatment begins with treating septic shock before it turns into MODS.
The goals of treatment include:
- Resuscitate the patient from septic shock, correct hypoxia, hypotension, and impaired tissue oxygenation.
- Identify the source of infection and treat it with antimicrobial therapy, surgery, or both.
- Maintain adequate organ system function, guided by cardiovascular monitoring, and interrupt the pathogenesis of MODS.
Addressing these goals involves:
- Early recognition of septic shock, which requires identifying signs of the systemic inflammatory response syndrome (SIRS) – mental changes, hyperventilation, hyperthermia or hypothermia, and an abnormal WBC count – along with the existence of a potential source of infection.
- Early cardiorespiratory stabilization and continued hemodynamic support
- Early and adequate antibiotic therapy
- Maintain blood glucose levels less than 150 mg/dL (milligrams per deciliter)
- Proper ventilator management with low tidal volume in patients with ARDS.
The road to recovery is often long and challenging for patients who survive sepsis and MODS. Patients may have physical, emotional, and cognitive consequences after discharge from the hospital. These patients also have a higher risk of repeat sepsis episodes. Aggressive rehabilitation programs, including psychological treatments, may be helpful.
Review
Now that we’ve learned all about MODS, let’s go over a few questions for review.
1. Organ failure that occurs as a result of the patient’s response to sepsis refers to
- SIRS
- Primary MODS
- Secondary MODS
- Septic shock
2. The scoring system used to assess the severity of organ dysfunction in patients who are critically ill from sepsis is called the
- BPP (Biophysical profile) Score
- SOFA (Sequential Organ Failure Assessment)
- AN (Care Assessment Need) Score
- GAF (Global Assessment of Functioning) Scale
That’s all for now! Thanks for watching and happy studying!
