End-Stage Renal Disease

Welcome to this video tutorial looking at end stage renal disease, also called end-stage kidney disease or kidney failure. If you haven’t seen it already, check out our video on ‘Acute kidney injury’, which gives an overview of kidney function and the acute disease. The kidneys filter waste and excess fluid from the blood, so when they fail, waste builds up and there is a gradual loss of kidney function, leading to chronic kidney disease. Chronic kidney disease progresses slowly over about 3 months and goes through 4 stages: kidney impairment, kidney insufficiency, kidney failure, and when only 10% of kidney function remains, end-stage renal disease.
The most common cause of end stage renal disease is diabetes and hypertension. Other problems that can cause kidney failure include autoimmune diseases, such as lupus; genetic diseases, such as polycystic kidney disease; nephrotic syndrome; and urinary tract problems.
Symptoms and Complications
Signs and symptoms of chronic kidney failure (CKF) result from imbalanced fluid and electrolytes, altered regulatory functions of the body, and retention of solutes. Anemia results from impaired red blood cell production. Patients may report lethargy, dizziness, and fatigue. Fluid and sodium balance is abnormal and may involve either abnormal retention or secretion of sodium and water; causing either high urine output or no urine output.
Other symptoms include:
- headache
- nausea & vomiting
- no appetite
- itching
- muscle cramps
- swelling in feet and ankles
- trouble catching breath
- insomnia
Chronic kidney failure affects all body systems.
Complications include:
- shock
- sepsis
- bleeding
- anemia
- hypertension
- hyperkalemia
- congestive heart failure
- pulmonary edema
- pericarditis
- atherosclerosis
- peptic ulcer disease
- peripheral neuropath
- bone density loss
- metabolic encephalopathy
The treatment for CKF also places the patient at risk for other complications. Hemodialysis often requires multiple hospital admissions for problems with vascular access devices including infection, clotting, or displacement of the catheter.
Renal failure is diagnosed using lab tests including serum creatinine levels and a 24-hr urinary creatinine clearance test, which both are essential in the evaluation of kidney function. A CBC would show decreased hemoglobin and hematocrit, and the blood chemistry shows electrolytes out of balance. Renal ultrasound will show the size and shape of the kidney, used to detect a mass, kidney stone, cyst, or other abnormality. A CT scan may be done to evaluate possible obstruction, preferably done without contrast due to the nephrotoxicity of the contrast agent.
Treatment Approaches
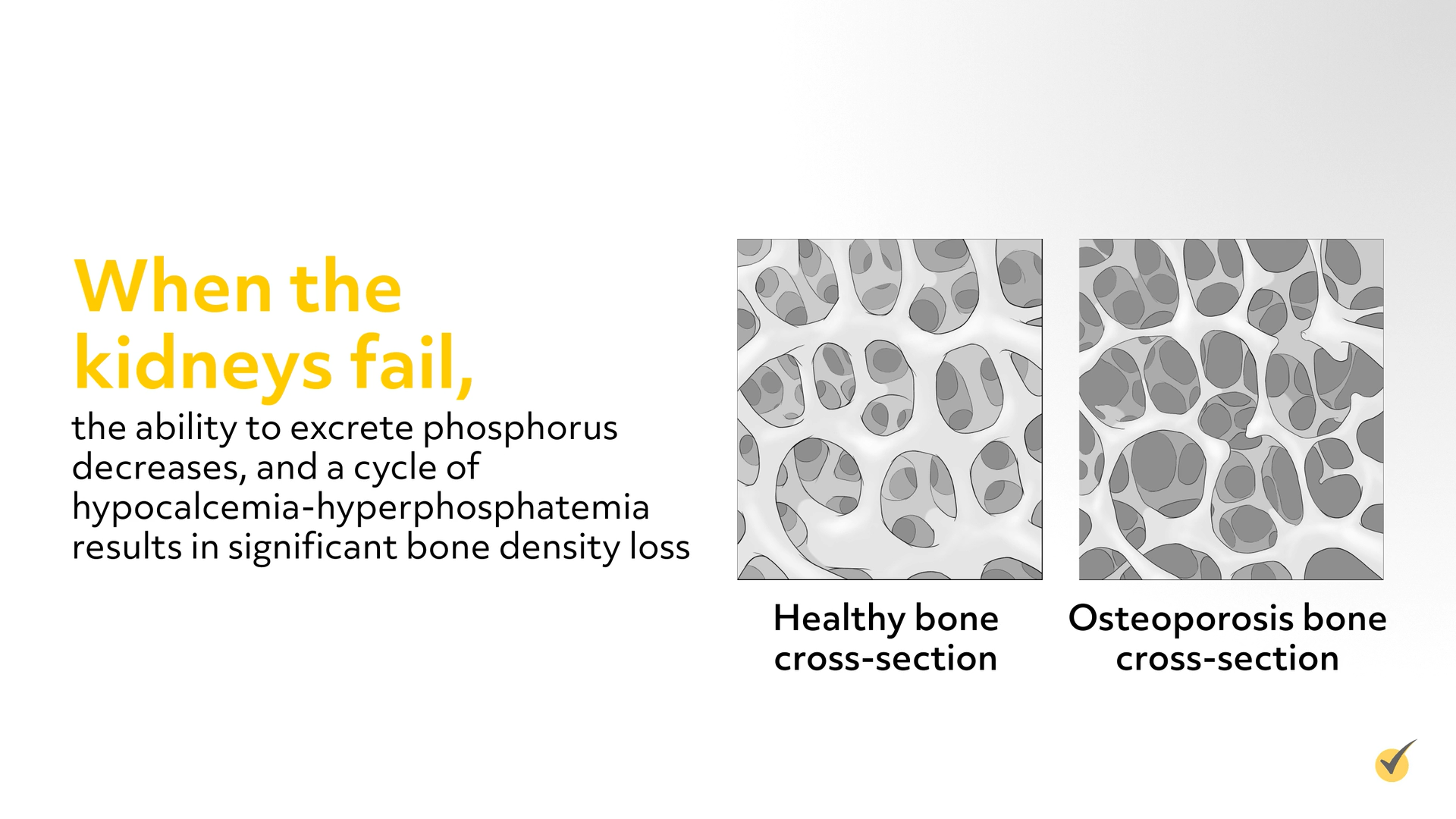
Treatment for chronic kidney disease focuses on stabilizing the internal environment by controlling fluid and electrolyte balance, preventing infection, controlling existing diseases, correcting anemia, and preventing complications. Metabolic acidosis occurs because the damaged kidneys are unable to excrete the normal load of acids generated by metabolism, and it is corrected by giving sodium bicarbonate. Hyperkalemia is treated with diuretic therapy or Kayexalate. When the kidneys fail, the ability to excrete phosphorus decreases, and a cycle of hypocalcemia-hyperphosphatemia results in significant bone density loss.
The goal of treatment is to decrease serum phosphorus levels by restricting phosphorus in the diet (eliminating dairy products and restricting protein), and giving phosphate binders (calcium carbonate and calcium acetate). Usually a reduction in phosphorus is associated with a small increase in serum calcium. Anemia universally accompanies chronic kidney failure, because there is insufficient production of erythropoietin by the diseased kidneys. Administering EPO, the recombinant form of human erythropoietin, increases hematocrit levels, decreases the need for blood transfusions, and improves energy levels. Most all patients receiving EPO also need iron supplementation due to the iron deficiency associated with chronic renal disease.
Dialysis and Transplantation
End stage renal disease is irreversible and requires dialysis or a kidney transplant to survive. Dialysis involves removing waste substances and fluid from the blood that are normally eliminated by the kidneys. It helps restore fluid and electrolyte balance, control acid-base balance, and remove waste and toxic material from the body. There are two types of dialysis: hemodialysis and peritoneal dialysis.
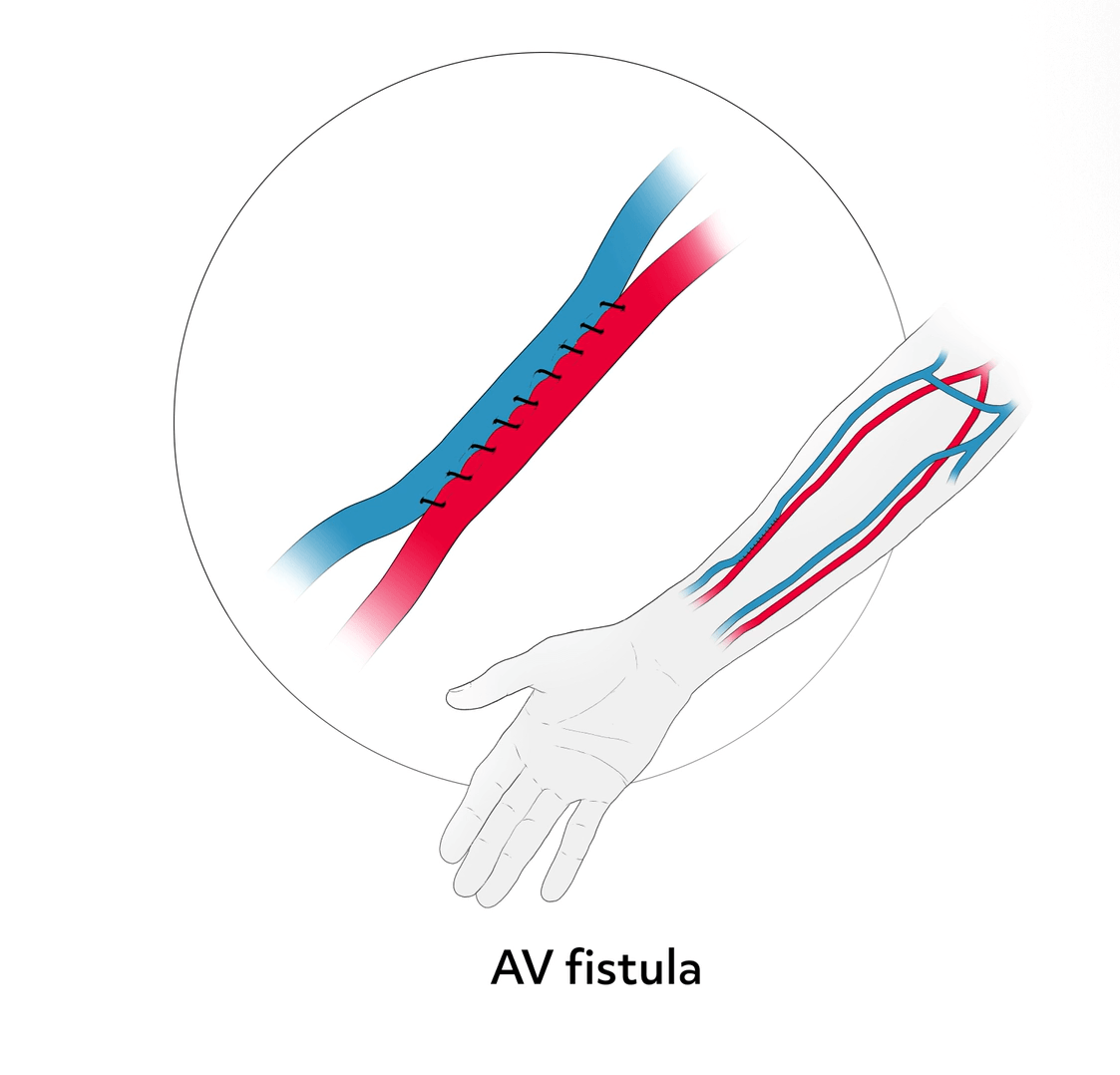
Hemodialysis involves moving the patient’s blood from the body, through a dialyzer in which diffusion and ultrafiltration occur, and then back into the patient’s circulation. Hemodialysis requires access to the patient’s bloodstream; the preferred choice being an arteriovenous fistula (AV fistula). This fistula is made by surgically joining an artery and a vein under the skin in the arm, which increases the pressure inside the vein, making the walls of the vein stronger. After about 3 to 4 months, the stronger vein has healed and can receive the needles used for hemodialysis. The fistula can then be used for many years.
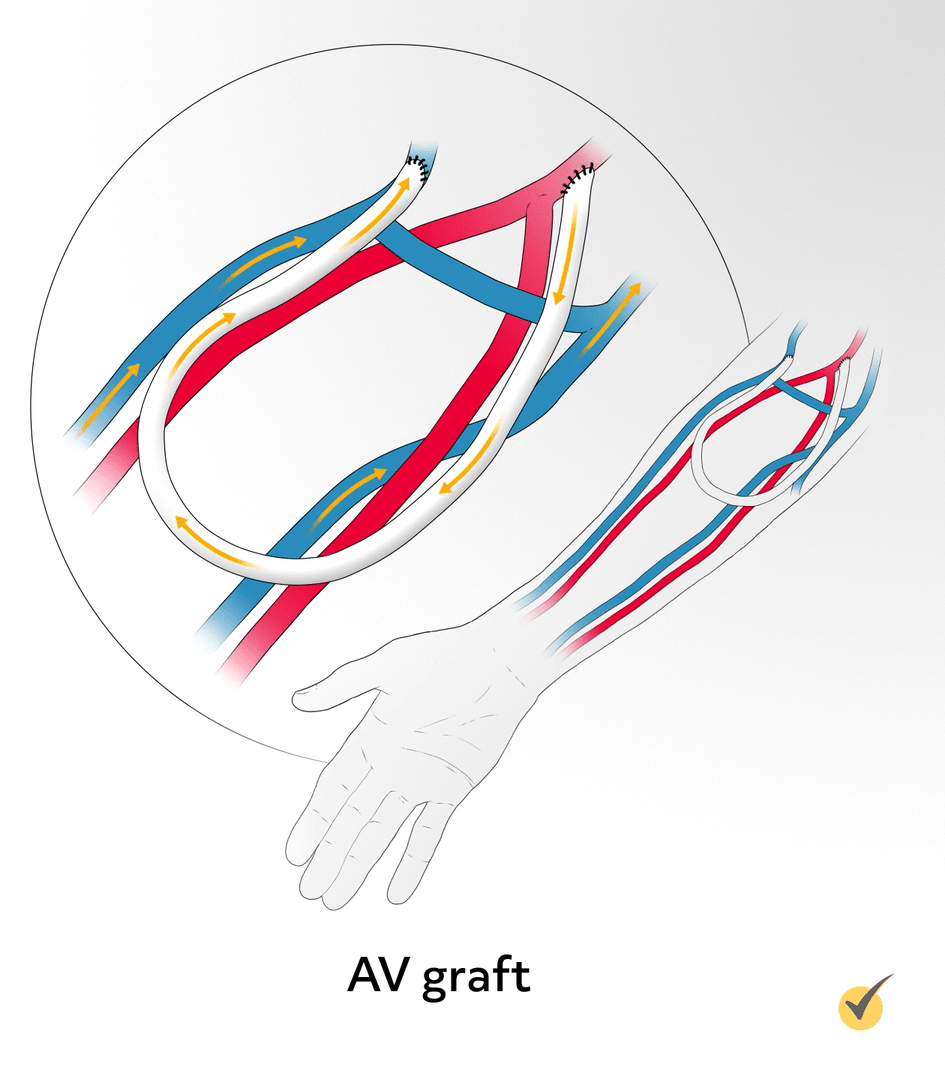
An arteriovenous graft (AV graft) is made by surgically joining the radial artery and a vein near the elbow with a plastic U-shaped tube, and it is usually ready to use about 3 weeks after the surgery. AV grafts are usually not as long lasting as AV fistulas, but can last several years if well cared for.
Temporary central venous catheters are placed in the internal jugular vein or femoral vein for dialysis while the AVF or AVG is healing. Hemodialysis is usually done several times a week and lasts for 4 to 5 hours. Possible complications include muscle cramps and sudden hypotension. Side effects can be avoided by following the proper diet and taking medications as prescribed.
Peritoneal dialysis involves instilling dialyzing fluid in the peritoneal cavity, with the peritoneum serving as the dialyzing membrane. A soft catheter is inserted in the lower abdomen near the navel, and approximately 2 liters of warm, sterile dialysate is infused into the peritoneal cavity over about 10 minutes. The fluid is left in the peritoneum for 20 to 30 minutes to absorb the waste products and toxins, then it is drained out by gravity. There are 3 different types of peritoneal dialysis: continuous ambulatory peritoneal dialysis (CAPD), continuous cyclic peritoneal dialysis (CCPD), and intermittent peritoneal dialysis (IPD). CAPD does not require a machine; the exchanges (passes) can be done 3 to 5 times daily during waking hours. CCPD requires the use of a special dialysis machine that can be used at home; it is done automatically, even while sleeping. IPD uses the same type of machine as the continuous cyclic, but treatments take longer. There are possible complications with peritoneal dialysis, including infection of the peritoneum, or peritonitis, which causes fever and stomach pain. There are several advantages to peritoneal dialysis, in that it provides a steady state of blood chemistry values, it can be used for patients who are hemodynamically unstable, and it is easily taught to patients, allowing them to dialyze at their convenience without the need for machinery.
Dialysis treatments are not cures for ESRD, but it will help the patient feel better and live longer. Another treatment option is kidney transplantation, which reverses many of the pathophysiologic changes associated with kidney failure. It also eliminates the dependence on dialysis and the need for dietary restrictions.
Diet therapy for patients with end stage renal disease must take into consideration lab results, nutritional status, and plans for dialysis, transplant, or no treatment. Limiting protein helps reduce waste buildup in the blood, however, protein intake must be adequate to avoid malnutrition. Potassium builds up in the body when kidney function declines, so it is best to avoid high potassium foods and monitor potassium levels regularly. Foods high in phosphorus should be avoided, due to phosphorus-calcium imbalance and bone changes that occur in chronic kidney disease. Fluid restriction and sodium restriction vary greatly with these patients, so it is helpful for the patient to be evaluated by a dietician.
Let’s go over a couple of questions for review…
Review Questions
Which of the following diagnostic studies is the most specific indicator of kidney function in a patient with renal disease? Choose all that apply
- Serum BUN
- Serum creatinine
- BUN/creatinine ratio
- 24-hour urinary creatinine clearance
Serum creatinine levels and a 24-hr urinary creatinine clearance test are both essential in the evaluation of kidney function.
Here’s another… Which of the following are signs and symptoms of end stage renal disease?
- Anemia, muscle cramps, & swelling in feet and ankles
- Insomnia, no appetite, & itching
- Fluid & sodium imbalance, & headache
- All of the above
All of the symptoms listed are symptoms of end stage renal disease.
Thank you for watching this video tutorial! Be sure to check out our other videos!
