Ventricular arrhythmias are abnormal heart rhythms that originate in the ventricles and are the leading cause of sudden cardiac death. In this video, you will learn about ventricular arrhythmias and how to identify them on an EKG strip.
Electrical Conduction of the Heart
Let’s look at a quick review of the heart’s electrical conduction system to understand how ventricular arrhythmias occur.
In a normal heartbeat, an impulse leaves the SA node, the heart’s natural pacemaker, signaling the atria to contract. It travels down the internodal pathways to the AV node then to the bundle of His, where it divides into right and left bundle branches, and onto the Purkinje fibers, causing the ventricles to contract.

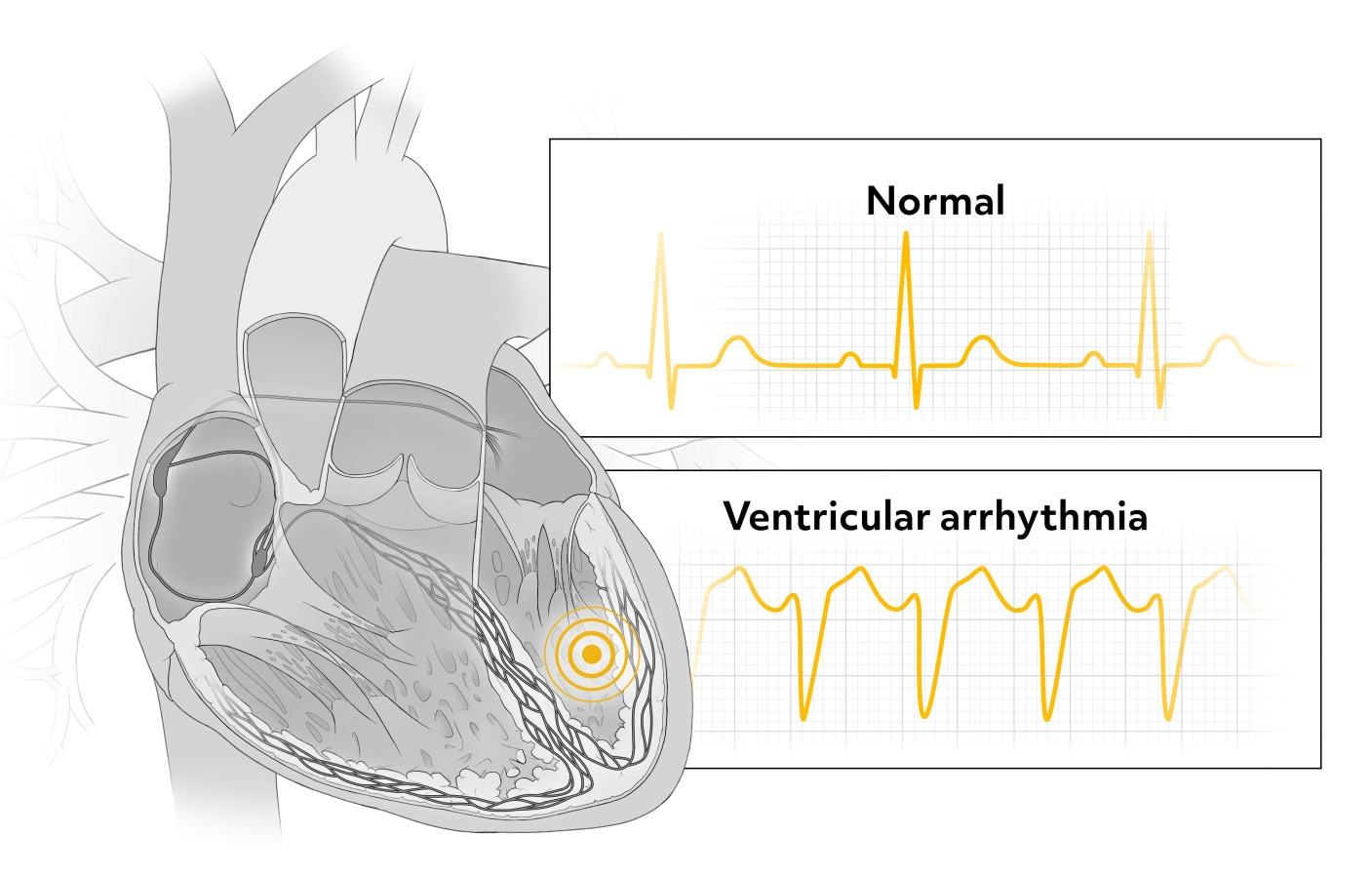
Problems arise when impulses vary from this normal pathway. When an impulse is generated by the ventricles, ventricular contractions are less effective and less efficient, resulting in decreased cardiac output.
Causes of Ventricular Arrhythmias
Factors leading to an impulse generated by the ventricles include:
- Myocardial ischemia, which is reduced blood flow to the heart
- Electrolyte imbalances, especially low potassium
- Hypoxemia
- Acidosis
- Drug overdose or toxicity
- Bradycardia
- Cardiomyopathy, which is a disease of the heart muscle
- Cardiac disease
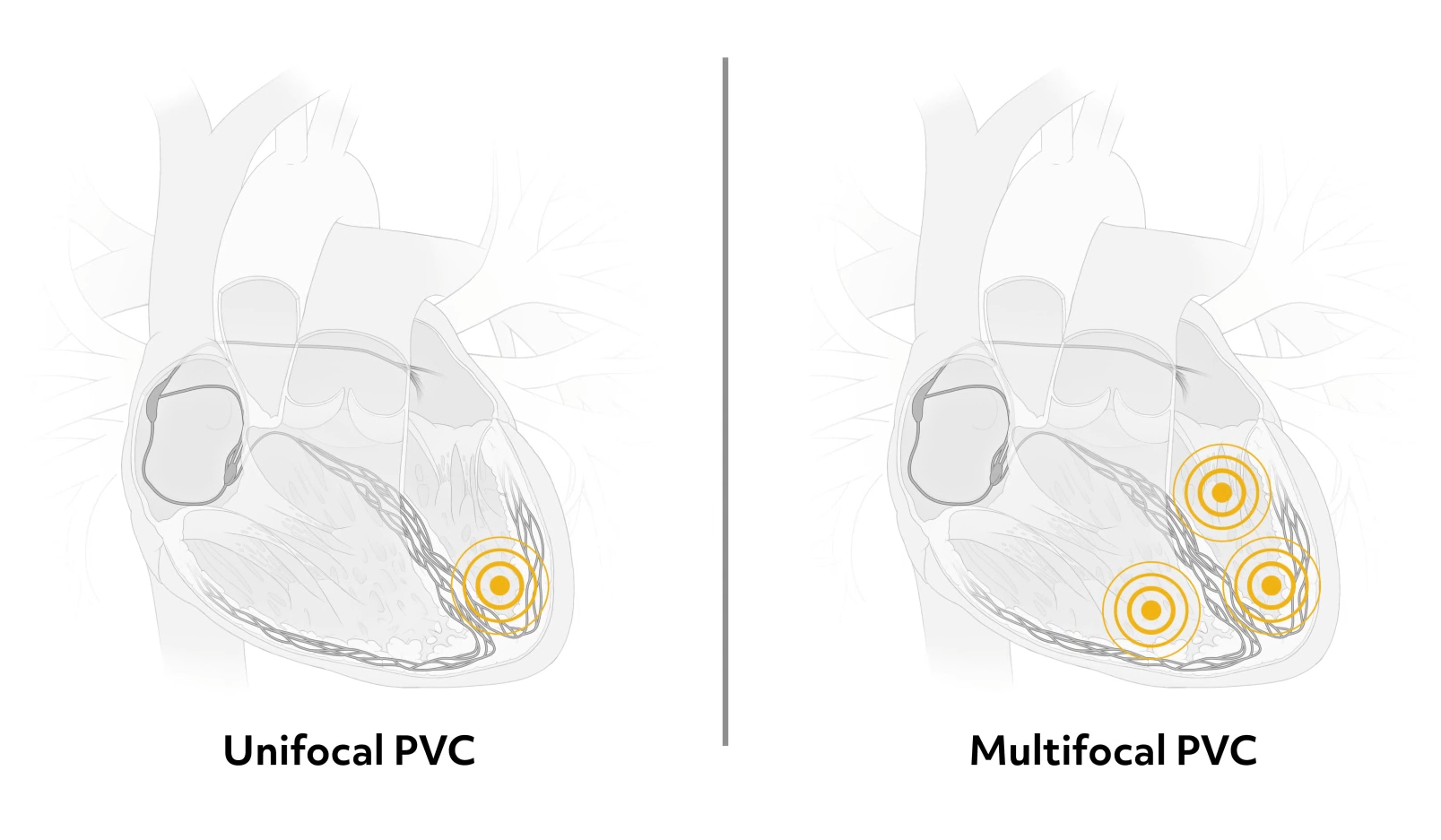
Ventricular arrhythmias can also occur in a healthy heart due to smoking, excessive caffeine, and other factors. A ventricular contraction occurs when an irritable cell and the ventricle fires and initiates an impulse. This is not part of the normal electrical cycle that starts at the SA node, but occurs prematurely or early in the cycle and is referred to as an ectopic beat, which is a disturbance in the cardiac rhythm.
Premature Ventricular Contractions (PVCs)
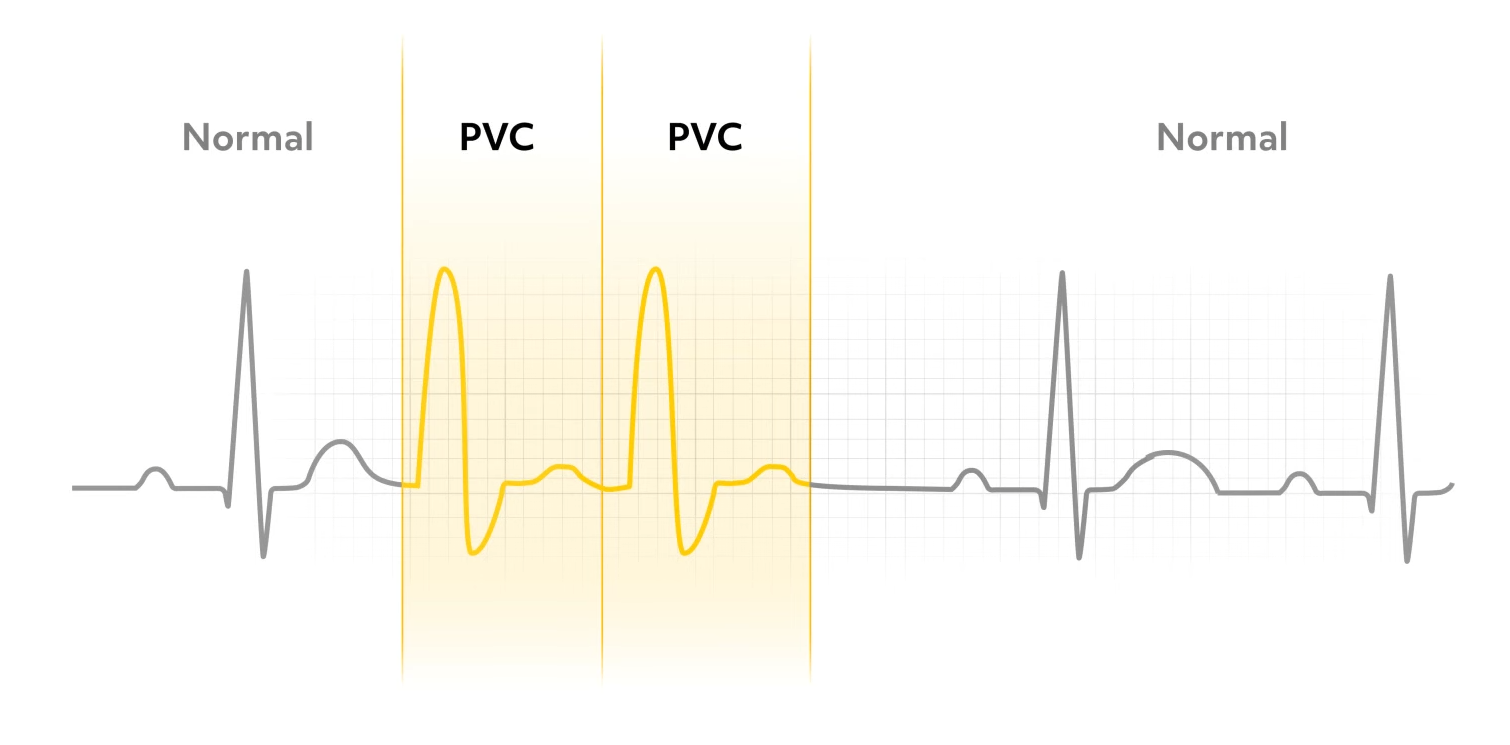
When initiated in the ventricles, the ectopic beat is further classified as a premature ventricular contraction, or PVC. PVCs have a characteristic wide and bizarre QRS. It’s usually greater than 0.12 seconds on the EKG. There is no associated P wave, and the T wave records in the opposite direction from the QRS.
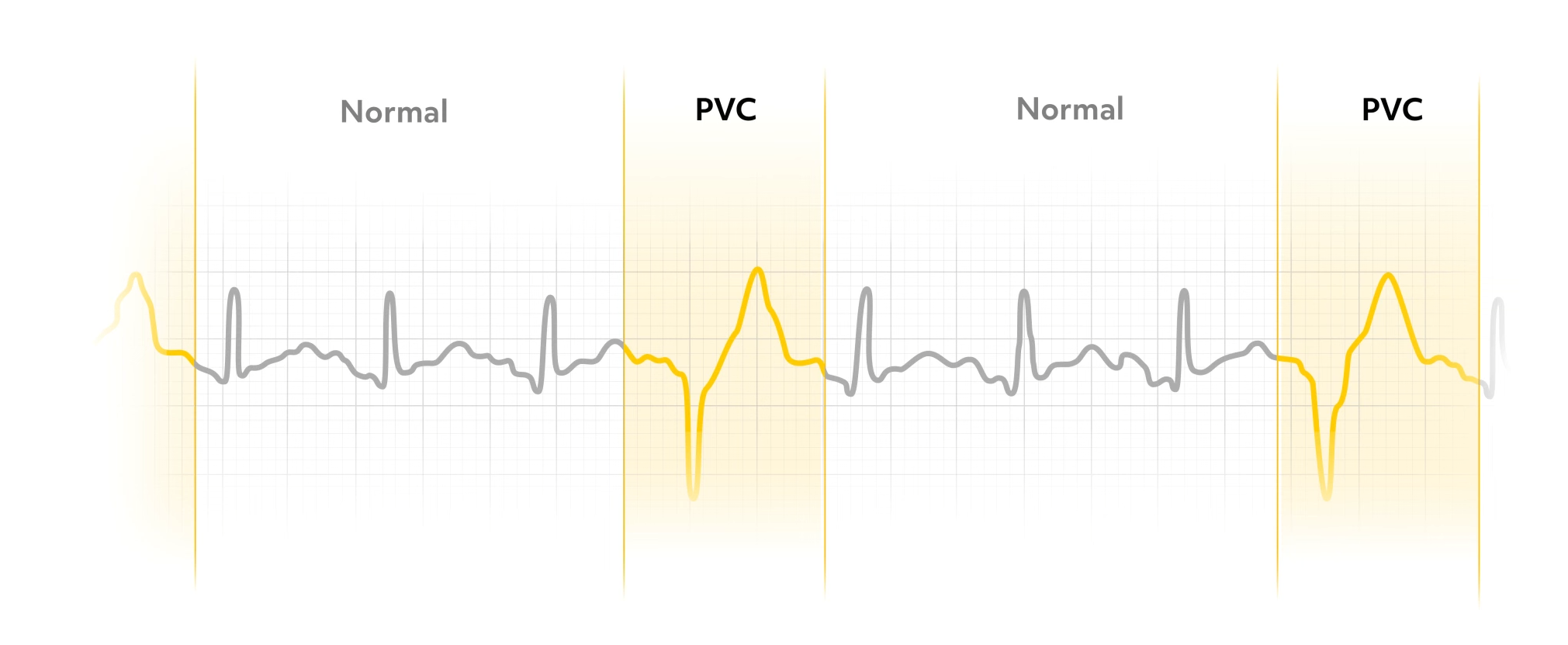
Most PVCs are followed by a pause until the next normal impulse originates in the SA node. PVCs can be unifocal, arising from the same irritable site in the ventricle, or multifocal, resulting from irritation in multiple cells and the ventricles.
Recognizing Dangerous PVCs
It is the nurse’s responsibility to watch for dangerous PVCs, which include PVCs occurring in groups of two or more, increasing frequency, such as increasing from 3-4 PVCs to 10-12 PVCs an hour later, or PVCs occurring near the T wave. The nurse will administer oxygen as ordered, check electrolyte levels, and give antiarrhythmic drugs if ordered.
Ventricular Tachycardia (V-Tach)
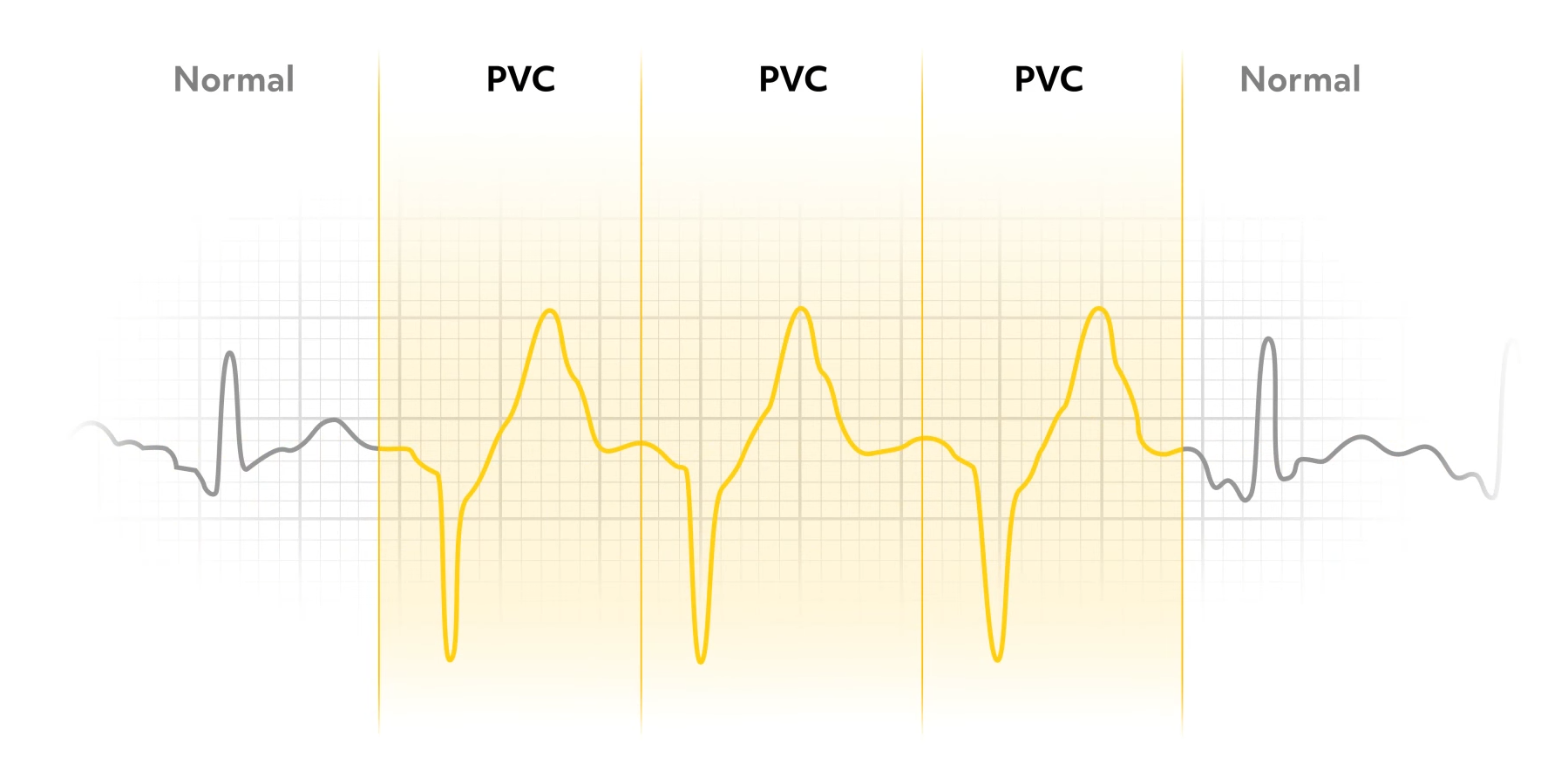
Three or more consecutive PVCs result in ventricular tachycardia, often referred to as V-Tach, which is a life-threatening arrhythmia. When the irritable cell in the ventricle fires repeatedly at a fast rate (usually 140-240 beats per minute), the SA node has lost control of the electrical conduction system. P waves may be present, but are not associated with the QRS complexes.

V-Tach is classified as sustained, which lasts more than 30 seconds, or nonsustained, in which the tachycardia stops before 30 seconds.
Treating V-Tach
Patients with V-Tach may have a pulse or they may be pulseless. The standard of care for pulseless V-tach is defibrillation to immediately convert the V-Tach to sinus rhythm and re-establish cardiac output and organ perfusion. If the patient is stable with adequate cardiac output, they generally receive antiarrhythmic drugs.
All drugs used to treat V-Tach decrease blood pressure. If the patient has unstable low blood pressure, the drug would further decrease cardiac output and organ perfusion.
Torsade de Pointes
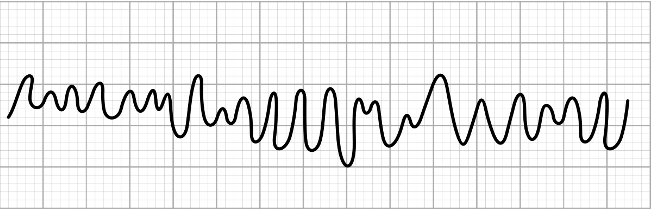
Torsade de pointes is a variation of V-Tach that can progress to ventricular fibrillation. A long QT interval commonly proceeds torsade de pointes. P waves, if seen, are not associated with QRS complexes. The QRS complexes are wide and bizarre, twisting along the baseline, and varying in size and direction.
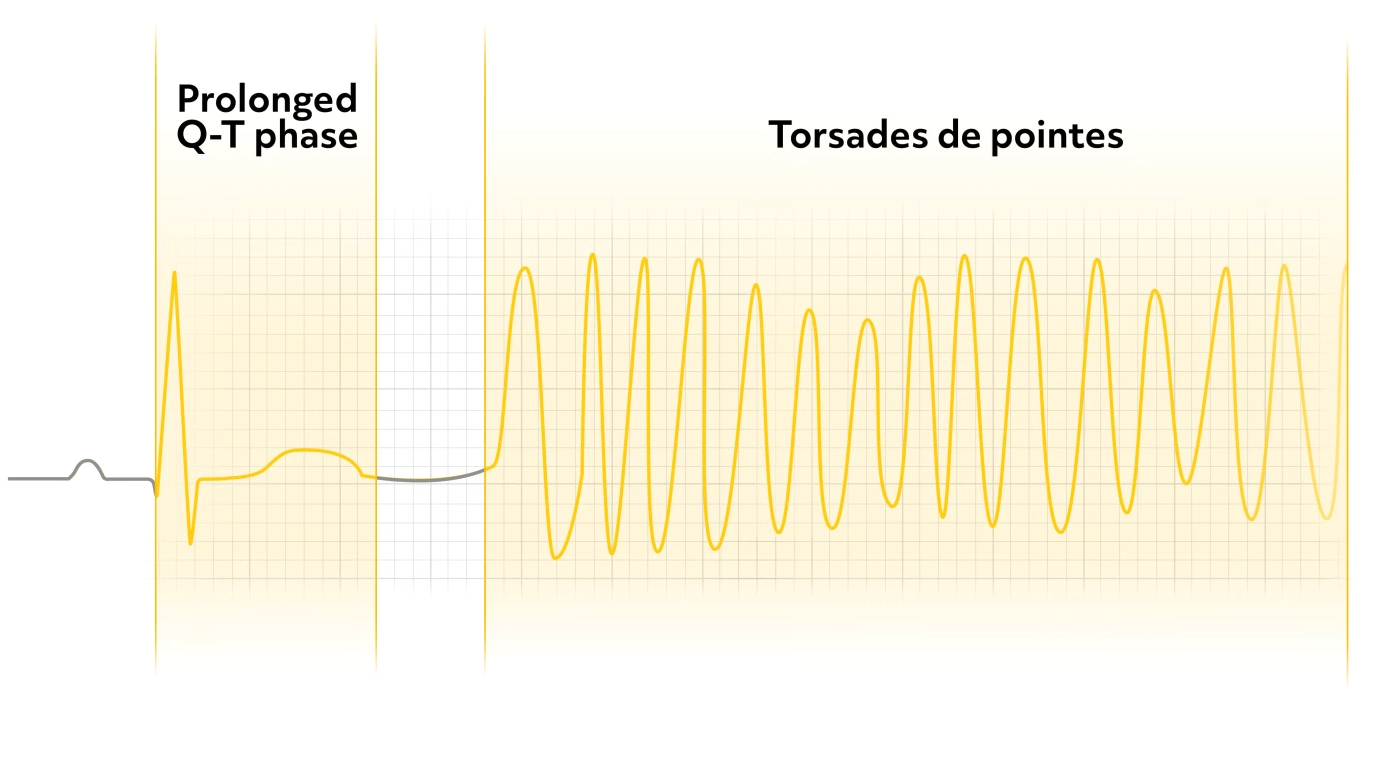
The unstable patient is defibrillated, as with pulseless V-Tach, then treatment is based on the cause of the arrhythmia.
Ventricular Fibrillation (VFib)
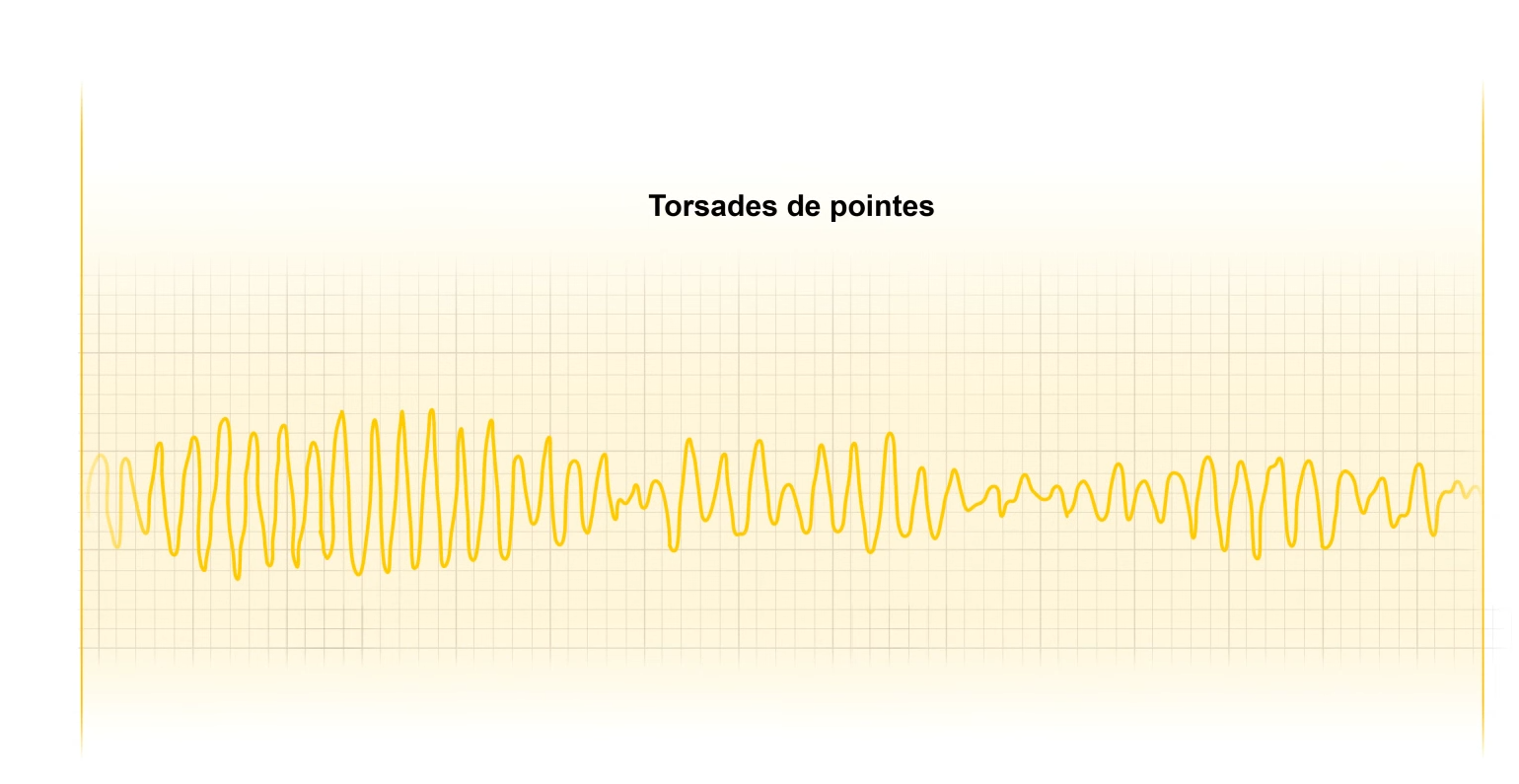
Ventricular fibrillation, or VFib is caused by uncoordinated quivering of the ventricles with no useful contractions.
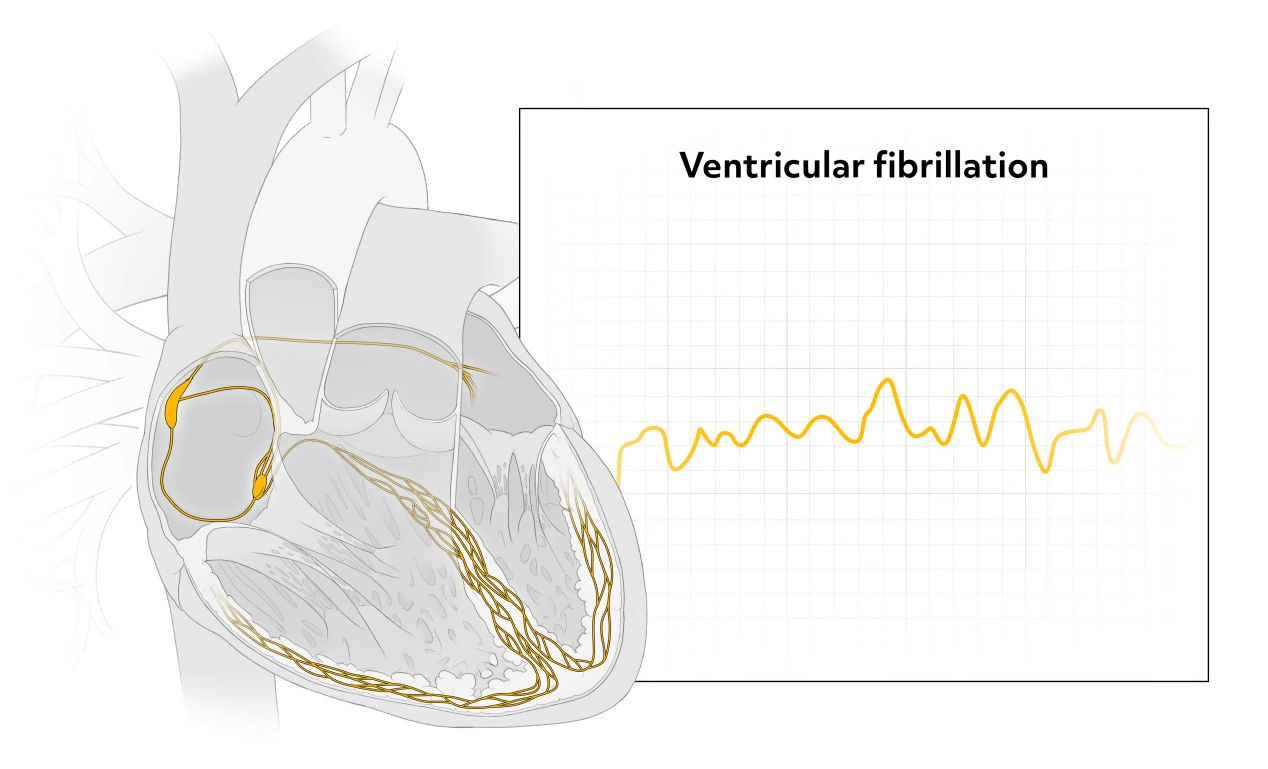
The ventricular activity of the heart is chaotic, and the EKG tracing consists of unidentifiable waves that represent an area of the heart depolarizing on its own. It causes immediate loss of consciousness and death within minutes, because the vital organs of the body, including the heart, are starved of oxygen.
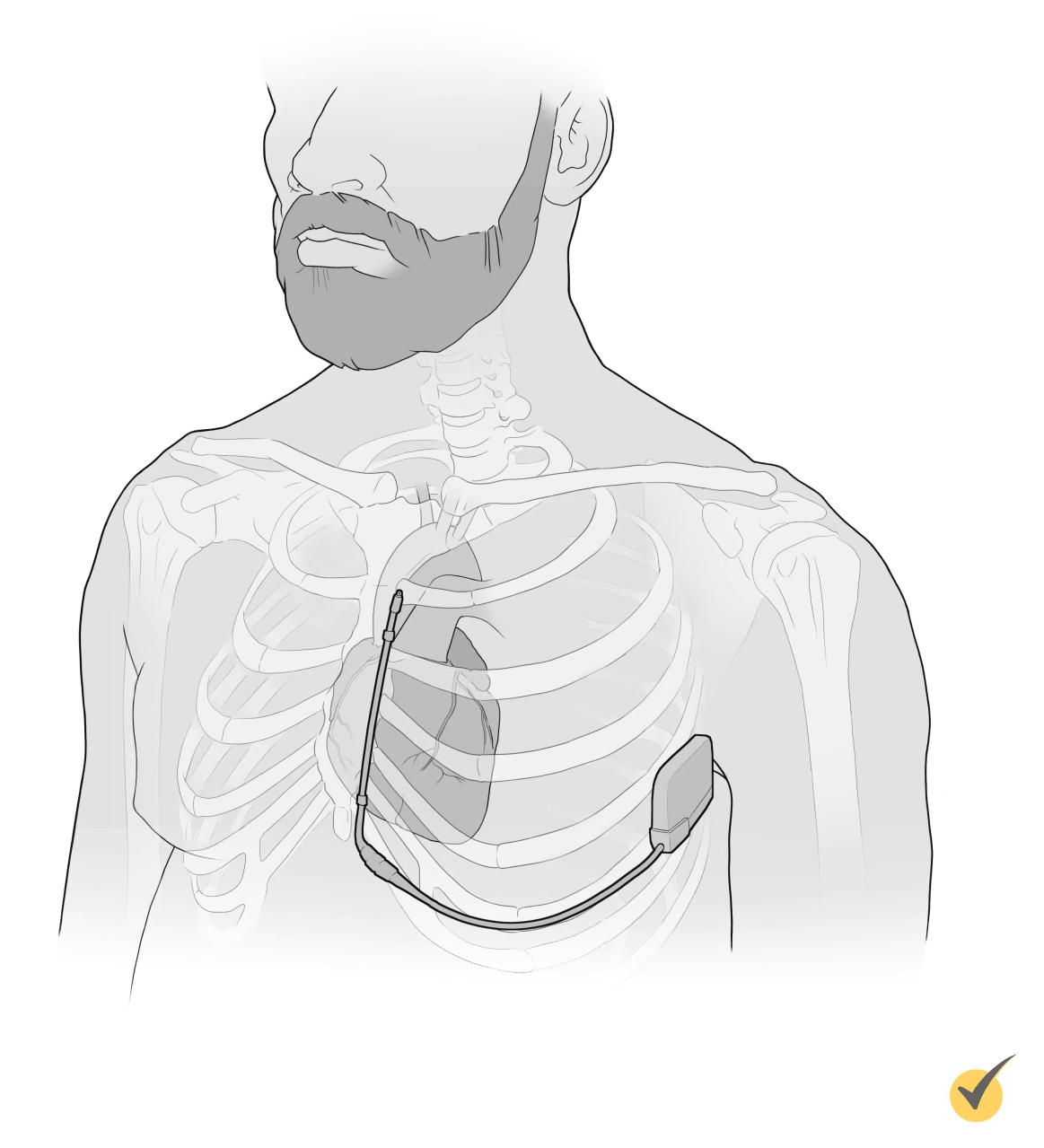
Defibrillation
The only way to stop fibrillation is with external electrical stimulation, or defibrillation, which must be performed immediately. Defibrillation depolarizes everything at once to allow the heart’s pacemaker, the SA node, to take control of the conduction system again. Automated external defibrillators, or AEDs, can be initiated quickly to allow for rapid defibrillation. While waiting for the AED, CPR can buy some time, but defibrillation is the most crucial treatment.
Remember, to treat the VFib, always defib.
It is recommended to give a single shock immediately followed by two minutes of CPR. Evidence shows that chest compressions after defibrillation produce more effective defibrillation. Since the heart is usually unable to produce effective cardiac output after a shock, the heart needs the supportive chest compressions to perfuse the body tissues. Chest compressions should also continue while the defibrillator is charging.
The treatment of choice for those that survive V-fib is an implantable cardioverter defibrillator, or ICD.
Review
Now let’s go over a few questions for review:
1. Ventricular arrhythmias result in:
- Increased cardiac output
- Decreased cardiac output
- An extra P wave on the EKG strip
- A shortened QRS complex on the EKG strip
When an electrical impulse is generated by the ventricles, ventricular contractions are less effective and less efficient, resulting in decreased cardiac output.
2. The standard of care for pulseless V-tach is:
- Antiarrhythmic drugs
- CPR
- Defibrillation
- None of the above
The standard of care for pulseless V-tach is defibrillation to immediately convert the V-tach to sinus rhythm and to re-establish cardiac output and organ perfusion. If the patient is stable with adequate cardiac output, they generally receive antiarrhythmic drugs.
3. A variation of V-tach that can progress to ventricular fibrillation is known as:
- Pulseless V-tach
- Sustained V-tach
- Nonsustained V-tach
- Torsade de pointes
That’s all for now. Thanks for watching, and happy studying!
Frequently Asked Questions
Q
What is a ventricular arrhythmia?
A
Ventricular arrhythmias are irregular rhythms that originate in the ventricles. In a healthy functioning heart, the impulses originate in the SA node of the right atrium, causing the atria to contract, which is then followed by the ventricular contraction. When impulses originate in the ventricles due to a compensatory mechanism or due to ventricular dysfunction, ventricular arrhythmias can occur.
Q
What is the most dangerous ventricular arrhythmia?
A
The most dangerous ventricular arrhythmia is ventricular fibrillation, or v-fib. Without immediate interventions, this rhythm is fatal.
Q
What is a PVC?
A
A PVC, or premature ventricular contraction, occurs when an impulse begins in the ventricles and conducts through them prior to the next sinus impulse. PVCs occur within an otherwise normal sinus rhythm. PVCs are characterized by an irregular heartbeat and an oddly-shaped QRS that is ≥0.12 seconds.
Q
What is ventricular tachycardia?
A
Ventricular tachycardia, or v-tach, is defined as greater than 3 PVCs in a row with a ventricular rate of 100 to 200 bpm. The rate, when a pulse is detectable, is regular with a wide, abnormally-shaped QRS complex.
Q
What is ventricular fibrillation?
A
Ventricular fibrillation, or v-fib, is a rapid, very irregular ventricular rate >300 bpm with no atrial activity observable on the ECG, caused by disorganized electrical activity in the ventricles. The QRS complex is not recognizable, as the ECG shows irregular undulations. There is no palpable pulse.
Q
What causes ventricular tachycardia and ventricular fibrillation?
A
Ventricular tachycardia and ventricular fibrillation are most often related to underlying coronary artery disease (heart disease, cardiomyopathy, myocarditis) or electrolyte imbalances.
Q
How is ventricular tachycardia treated?
A
V-tach with a pulse is treated with synchronized cardioversion (if the patient is unstable) or adenosine (6 mg rapid IV push followed by a flush of normal saline). V-tach without a pulse should be treated with defibrillation and epinephrine (1 mg IV push every 3 to 5 minutes) and amiodarone (300 mg IV push followed by 150 mg IV push). The underlying cause should be treated.
Q
How is ventricular fibrillation treated?
A
V-fib should be treated with defibrillation and epinephrine (1 mg IV push every 3 to 5 minutes) and amiodarone (300 mg IV push followed by 150 mg IV push). The underlying cause should be treated.
Q
What does the EKG for a PVC look like?
A
The EKG for a PVC looks like: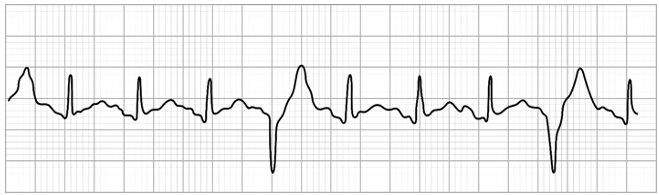
Q
What does the EKG for ventricular tachycardia look like?
A
The EKG for ventricular tachycardia looks like: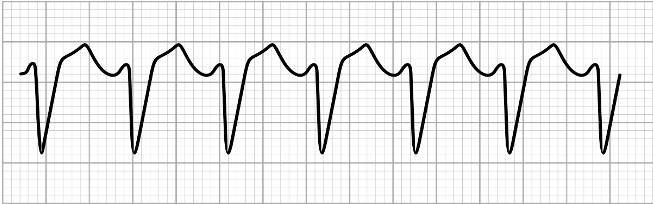
Q
What does the EKG for ventricular fibrillation look like?
A
The EKG for ventricular fibrillation looks like: