
Welcome to this video tutorial on the complications of diabetes.
Diabetes is a group of metabolic diseases characterized by hyperglycemia (high blood sugar) that results from defects in insulin secretion, insulin action, or both, and affects multiple systems of the body.
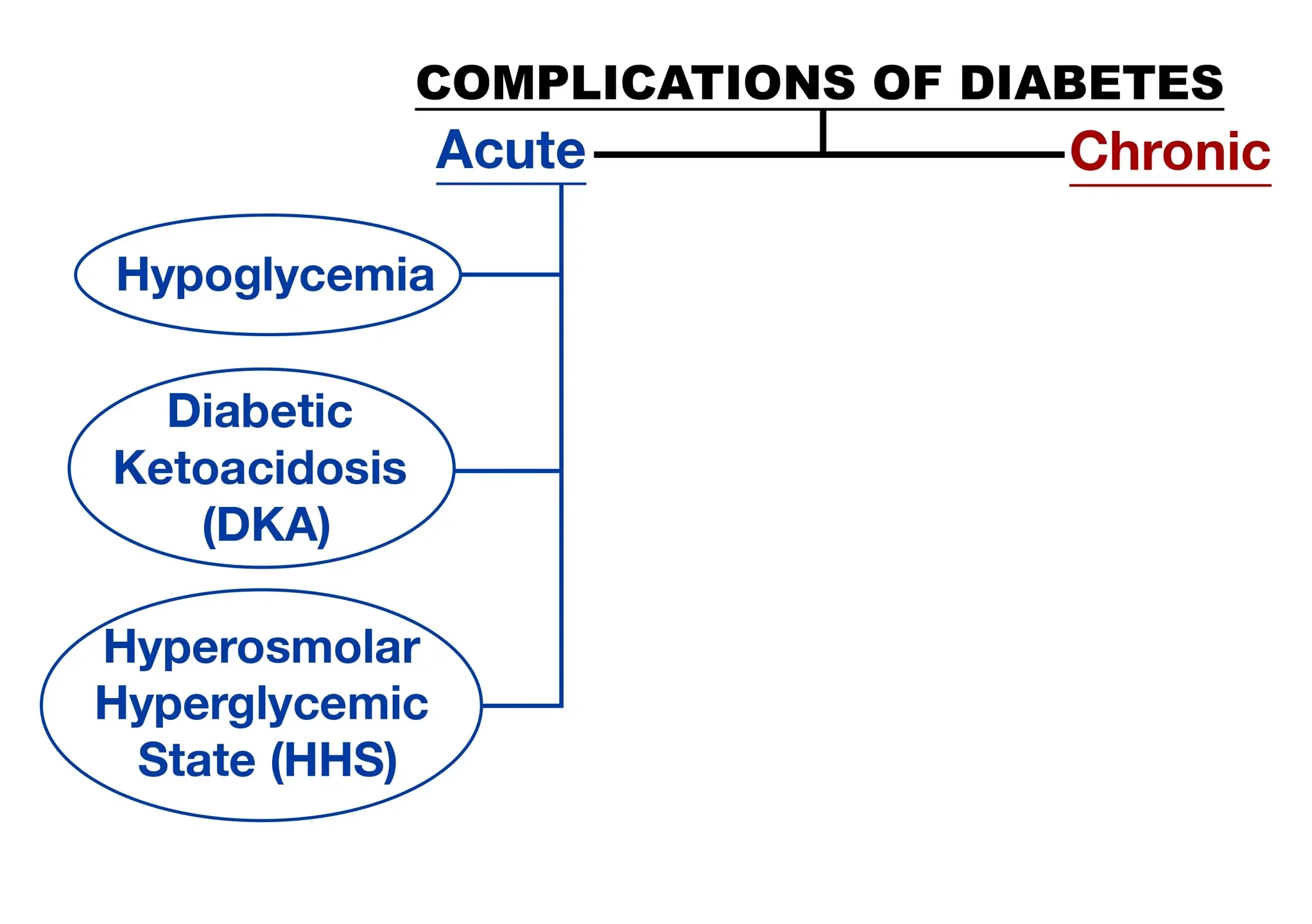
Uncontrolled diabetes can cause metabolic imbalance leading to acute complications, requiring immediate medical attention. Ongoing hyperglycemia will then develop into chronic complications.
Acute Complications
Let’s start by looking at the acute complications that require immediate medical intervention.
Hypoglycemia
Hypoglycemia, or a blood glucose level of less than 60 mg/dL, is a potential complication of insulin therapy or oral hypoglycemic agents. It can also be caused by skipping a meal, inconsistent carbohydrate intake, over-exercising, or alcohol consumption.
Common signs and symptoms of hypoglycemia may be adrenergic (caused by activation of the sympathetic nervous system) or neuroglycopenic (which is caused by depression of central nervous system activity as the brain receives an insufficient supply of glucose). Adrenergic symptoms usually result from a rapid drop in glucose and occur first, including being pale, sweaty, having tachycardia, palpitations, nervousness, irritability, feeling cold, weak, trembling, and hungry.
The particular signs and symptoms vary depending on the blood glucose level, how fast the glucose level dropped, and the duration of hypoglycemia. When the hypoglycemia is slow-developing, as with long-acting insulin or with oral hypoglycemic agents, the central nervous system signs and symptoms predominate. Those signs include headache, mental confusion, numbness around mouth, incoherent speech, double vision, fatigue, emotional lability, convulsions, and coma.
If a rapid drop in blood sugar occurs and is allowed to persist, both the sympathetic and central nervous system signs usually occur.
The diabetic patient should be educated about recognizing signs of hypoglycemia and how to treat it. As long as the patient is conscious, they should self-treat with 15 g of quick-acting carbohydrate, such as 4 oz of juice (no added sugar), 3-4 glucose tablets, or 3 hard candies. Recheck the fingerstick blood glucose in 15 minutes and if it remains below 60, the patient should self-treat again. In an unconscious patient, never try to give oral glucose.
In the hospital setting, one ampule of 50% dextrose is given IV push. In the outpatient setting a friend or family member can inject 1mg of glucagon subcutaneously, which causes the liver to release its glycogen store. The patient will usually regain consciousness within 10-20 minutes, and should then eat a snack of 45g carbohydrates to aid in replacing glycogen stores. Patients are often nauseated after receiving glucagon and may vomit. When hypoglycemia is severe, seizures may also occur.
Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is another serious acute complication when excess blood acids, called ketones, build up in the body. Ketones are formed when the body burns fat for fuel instead of glucose. This can occur when there is not enough insulin in the body to process sugars.
DKA is triggered by illness or not taking insulin. The progressive hyperglycemia causes glucose to spill out into the urine, resulting in water and electrolyte losses, causing dehydration and an increase in thirst. The lack of insulin and corresponding elevation of glucagon leads to increased release of glucose by the liver as well as ketone bodies, which are acidic and must be cleared from the circulation.
DKA can occur in patients with type 1 or type 2 diabetes, but it’s rare with type 2. Risk for DKA is increased with type 1 diabetes, under age 19, stress, physical or emotional trauma, high fever, heart attack, stroke, smoking, or drugs/alcohol. Signs and symptoms of DKA include high blood sugar levels, high levels of ketones in urine, fruity smelling breath, flushed face, nausea and vomiting, abdominal pain, rapid deep gasping breaths, frequent urination, extreme thirst, dry mouth and skin, weakness, confusion, and loss of consciousness. If left untreated, DKA can lead to coma or death. Treatment involves rehydration with IV fluids, insulin therapy, and electrolyte replacement.
HHNS
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) has some similarities to DKA, but is an acute complication of type 2 diabetes. The differences include profound dehydration, with fluid deficit as high as 8-9 liters. Blood sugar levels are higher, with serum glucose levels in the range of 600 to 2000.
Ketosis is absent because patients with type 2 diabetes have insulin secretion to prevent ketosis. The kidneys try to get rid of the extra blood sugar by putting more glucose into the urine, which increases urination and loss of body fluid, causing dehydration. Dehydration makes the blood thicker and the blood sugar level is too high for the kidneys to be able to fix.
This also causes an imbalance of minerals in the blood, especially sodium and potassium. This imbalance of fluids, glucose, and minerals in the body can lead to severe problems, such as brain swelling, abnormal heart rhythms, seizures, coma, or organ failure. Without rapid treatment, HHNS can cause death. Primary treatment involves IV rehydration, which resolves the hyperglycemia, so IV insulin is usually not needed.
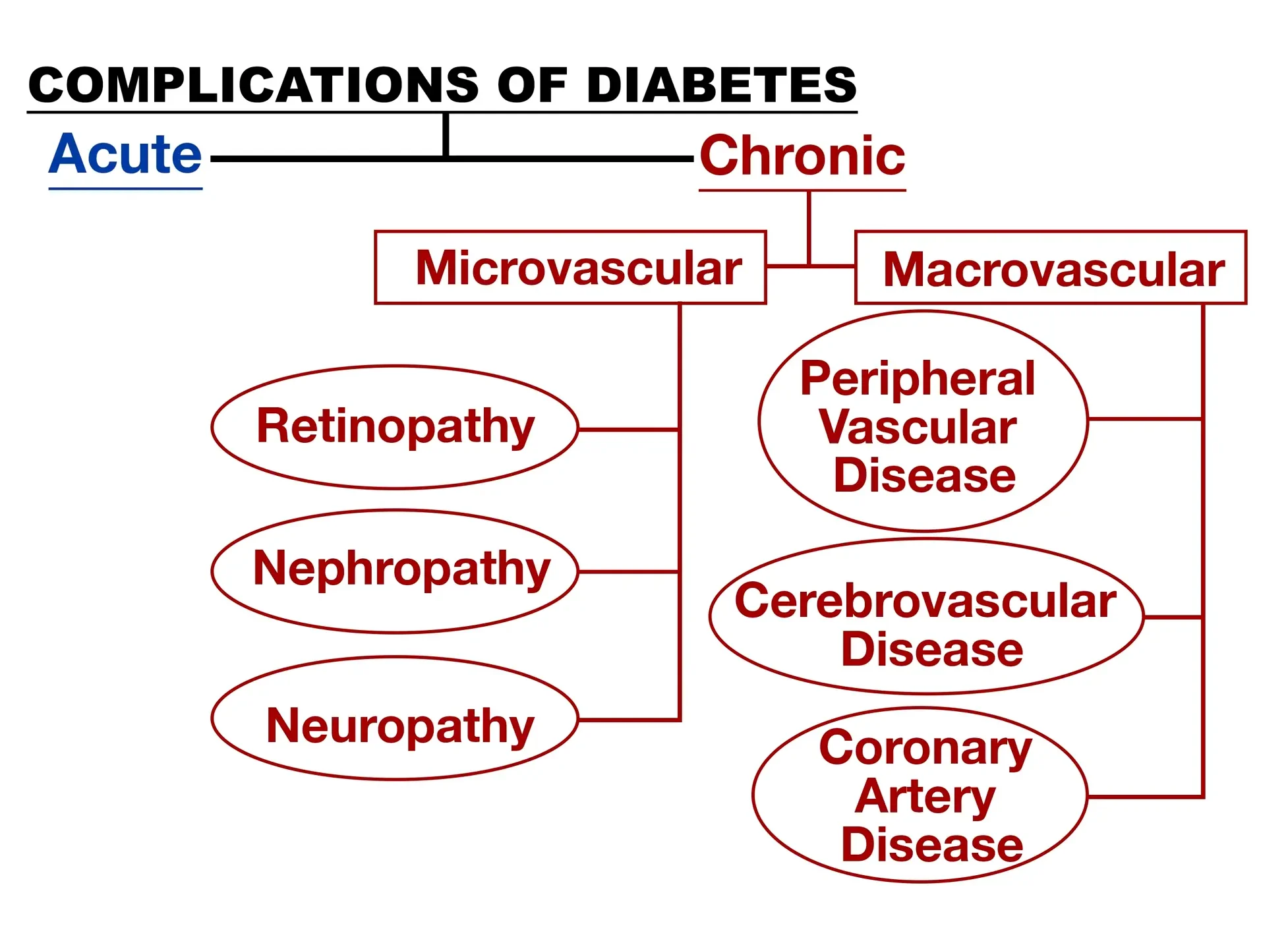
Chronic Complications
Ok, now let’s look at the chronic complications of diabetes, that develop from ongoing hyperglycemia. They are classified as microvascular or macrovascular. These complications are a result of the length and degree of hyperglycemia.
Microvascular Complications
Microvascular complications affect the smaller blood vessels, such as the eyes (leading to diabetic retinopathy), kidneys (leading to diabetic nephropathy), and nerves (leading to neuropathy). The effects of high blood glucose as well as high blood pressure can damage eye blood vessels, causing retinopathy, cataracts and glaucoma.
Diabetic retinopathy is the leading cause of new blindness among adults 20 to 74 years old in the United States. High blood pressure also accelerates the development and progression of retinopathy.
Diabetic nephropathy is the leading cause of end-stage renal disease in the US, with 20% of all diabetic patients having nephropathy. Excess blood glucose overworks the kidneys and high blood pressure damages the small blood vessels.
Microscopic amounts of albumin in the urine is the earliest lab abnormality, which may then progress to albuminuria (clinical proteinuria). Aggressive blood pressure control lessens the albuminuria, decreases the rate of deterioration of the kidneys, and improves survival.
Diabetic neuropathy affects 60%-70% of diabetic patients, and involves damage to nerves in the peripheral nervous system. The most common symptoms involve numbness in the legs or feet; but depending on the nerves affected, it can also cause shooting pains; problems with the digestive system, urinary tract, blood vessels, and the heart.
Microvascular disease may also impair skin healing, so that even minor breaks in skin can develop into a major infection and deep ulcer, especially in the lower extremities. Control of blood glucose can prevent or delay many of these complications, but may not reverse them once established.
Macrovascular Complications
Macrovascular complications involve atherosclerosis of large blood vessels, such as those supplying the heart, brain, and extremities. This can lead to angina, myocardial infarction, transient ischemic attacks, strokes, and peripheral arterial disease.
Cardiovascular disease is two to four times more prevalent in diabetic patients and is responsible for approximately 75% of diabetes-related deaths. Diabetic foot syndrome is common among diabetics due to the atherosclerosis of the blood vessels to the extremities. It results from three factors: neuropathy, ischemia, and sepsis. Loss of sensory nerves in the feet leads to painless trauma and potential ulcer formation.
The lack of blood supply (ischemia) results in slower healing and possible sepsis. These events can result in gangrene and ultimately amputation. Blood sugar control is so important, as well as IV antibiotics to limit the spread of infection. Foot care is an important aspect of diabetic teaching, with proper toenail trimming and the use of orthotic shoes to prevent ongoing trauma associated with diabetic foot.
Immune dysfunction is another major complication, developing from the direct effects of hyperglycemia on cellular immunity. Therefore, diabetic patients are especially susceptible to bacterial and fungal infections.
In order to prevent and avoid the complications associated with diabetes, achieving and maintaining adequate control of blood sugar, diet, exercise, medications, monitoring, and education is a must.
Review Questions
Let’s go over a couple of questions for review:
1. A patient presents with a blood glucose of 425, positive ketones in their urine sample, weakness, vomiting, and fruity smelling breath. What complication of diabetes are they exhibiting?
- Hypoglycemia
- Nephropathy
- Diabetic Ketoacidosis
- Hyperosmolar Hyperglycemic State
Those are all signs and symptoms of the acute complication of DKA.
2. Microvascular chronic complications include which of the following?
- Diabetic retinopathy and peripheral vascular disease
- Diabetic nephropathy and diabetic neuropathy
- Cerebrovascular disease and coronary artery disease
- All of the above
Microvascular complications affect the smaller blood vessels leading to neuropathy, nephropathy, and retinopathy.
Thank you for watching this video about the complications of diabetes!
