
Hi, and welcome to this video on chronic insomnia.
Sleep Disorders
While there are individual differences in a person’s need for sleep and their sleep-wake patterns, both of which change as we age, adequate sleep is vital for optimal health and well-being. Several internal factors (circadian rhythms and sleep homeostasis) and external factors (e.g., noise, light, extreme temperatures, stress, and medications) affect the quality of your sleep and how much sleep an individual gets each night.
Many individuals experience occasional sleep-related problems, with a prevalence as high as 70% of US adults reporting insufficient or poor sleep at least one night a month. However, when sleep-related difficulties occur on a regular basis and are accompanied by daytime symptoms that interfere with the person’s functioning, a sleeping disorder may be suspected.
Sleep disorders are a heterogeneous group of conditions that chronically affect the quantity, quality, and/or the timing of sleep. There are over 90 different diagnosable sleep disorders and three different methods (nosology systems) currently used to classify them: the Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM–5), the International Classification of Sleep Disorders 3rd edition (ICSD-3), and the International Classification of Diseases, 10th Edition, Clinical Modification, ICD-10-CM.
Regardless of the classification method, each group of sleep disorders has common causes, distinct characteristics, and similar treatment regimens. Despite the differences in the etiology and characteristics, most sleep disorders, including insomnia, have at least one of the following consequences that either cause distress or hinders daytime functioning:
- Excessive daytime sleepiness;
- Fatigue, general tiredness, or reduced energy;
- Poor attention or concentration, as well as impaired memory and learning;
- Slowed reaction time, impaired judgement, and diminished problem-solving abilities;
- Irritability, anxiety, difficulty controlling emotions;
- Impulsivity, aggression, and hyperactivity.
Prevalence and Impact
Sleep disorders have a widespread deleterious effect on human health and negatively impact nearly every key indicator of public health, including: health care utilization rates, accident and injury rates, morbidity rates, and mortality rates.
Insomnia is the most common sleep disorder- commonly affecting older adults, especially post-menopausal women, shift workers, and those with chronic medical and mental health comorbidities, especially depression. Additionally, those who have a parent, sibling, or child with insomnia are at greater risk of developing insomnia, and individuals with a history of insomnia are at high risk for a reoccurrence. The more risk factors an individual has, the greater the risk of developing insomnia. However, it is possible for an individual with no risk factors to develop insomnia.
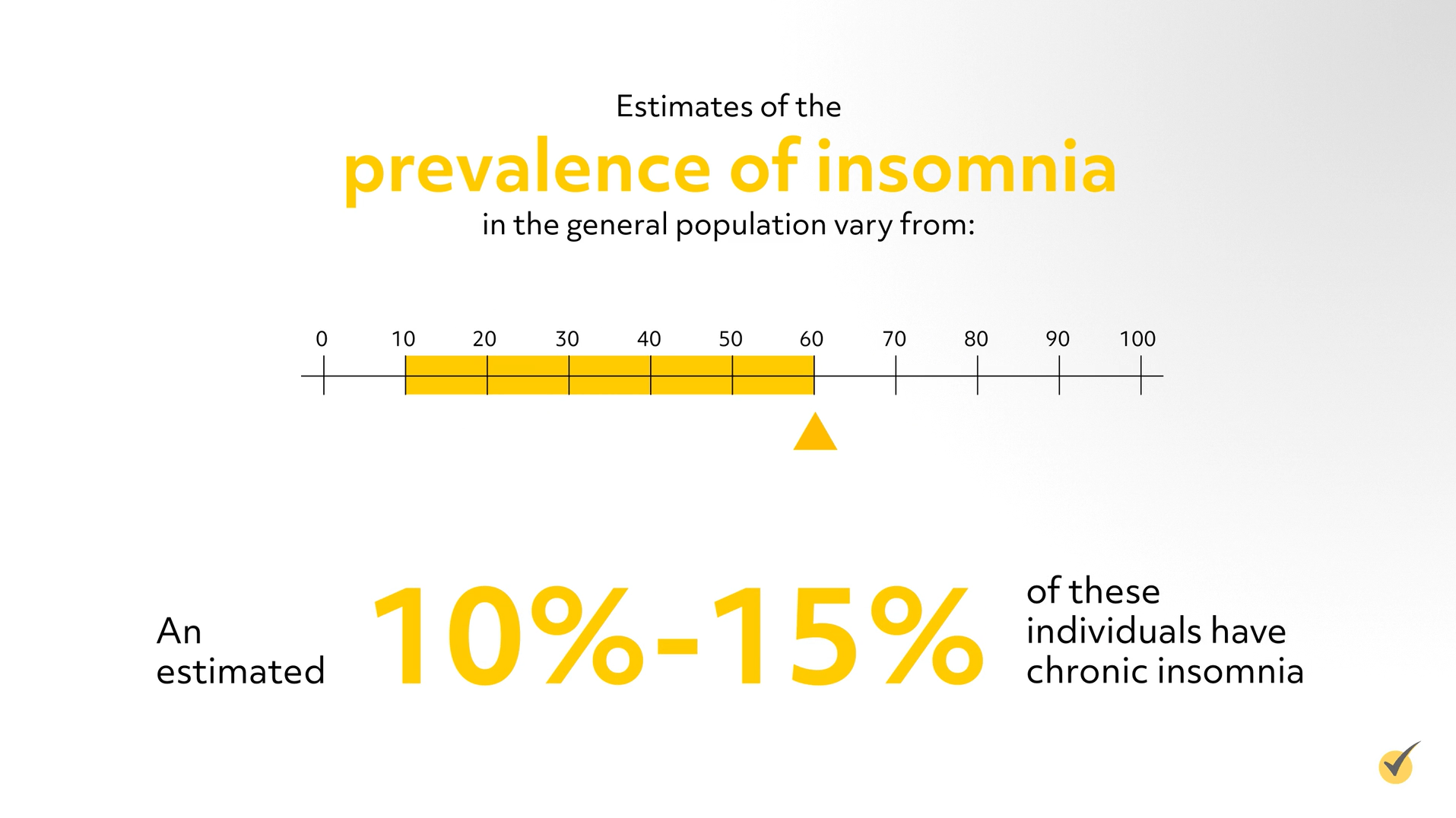
Insomnia occurs in both genders and individuals of all ages and is widespread, occurring in all races and ethnic groups. Estimates of the prevalence of insomnia in the general population vary from a reported low of 10% to a high of 60%. An estimated 10%-15% of these individuals have chronic insomnia. Despite its negative impact on daytime functioning, insomnia symptoms often go unreported. Additionally, in adults with insomnia who have reported their difficulties with sleep, more than two-thirds (72.2%) stated that their health care provider failed to recognize, diagnose, and treat their condition.
Diagnosing Insomnia
Insomnia is characterized by a repetitive difficulty with one or more of the following symptoms:
- difficulties falling asleep:
- trouble staying asleep (frequently waking during sleep);
- inability to return to sleep after nocturnal awakenings; and
- waking up earlier than desired with an inability to fall back asleep.
- These symptoms are not explained or attributed to another sleep-wake disorder, medical or psychiatric condition, or the physiological effects of medication or a drug of abuse.
The number of these sleep symptoms vary from person to person, and, while a person may only experience one type of symptom, it is not unusual for a person to experience multiple symptoms at the same time or for the number and type of symptoms to vary over time.
Insomnia is primarily diagnosed by careful physical and mental status examination, a comprehensive review of an individual’s medical history; and a thorough diagnostic interview regarding the individual’s pre-sleep habits, sleep environment, sleep-wake patterns, and specific sleep related complaints. Standardized interview tools for the clinical evaluation of insomnia include: The Sleep Disorders Interview; the Insomnia Screening Questionnaire; and the Structured Clinical Interview for Sleep Disorders (SCISD).
While there is no definitive diagnostic test for insomnia, the clinician can use a variety of tests and tools to assess the quality and duration of an individual’s sleep. These include:
Sleep questionnaires – These questionnaires summarize the individual’s perception of their own sleep quality. Examples include: Pittsburgh Sleep Quality Index (considered the gold standard of self-reported assessments), Epworth Sleepiness Scale, Insomnia Severity Index, and Sleep Quality Scale.
A sleep diary – is a self-reported record of an individual’s sleep patterns, sleeping habits and daytime activities that can impact sleep. Usually collected over a period of several weeks, it is the most important method of evaluating a sleep-wake complaint. Multiple versions are available, and it is important to choose a sleep diary appropriate for clinical practice. Examples of sleep diaries include: Consensus Sleep Diary, Pittsburgh Sleep Diary, and National Sleep Foundation Sleep Diary.
Symptom checklists, psychological screening tests, and quality of life questionnaires are used to clarify the cause, pinpoint symptoms, and aid diagnosis. The individual’s presentation guides the choice of tool. Examples include:
- The Sleep Disorders Symptom Checklist,
- Hopkins Symptom Checklist-90,
- Patient Health Questionnaire-9,
- Sleep-Hygiene Checklist, and;
- The Dysfunctional Beliefs About Sleep (DBAS) Questionnaire.
Bed partner or caregiver interviews also assist in gathering data about the individual’s sleep.
Actigraphy is used to assess sleep-wake cycles over a period of time; using a device called an actigraph, which monitors and records movement.
While hyperarousal, an abnormal state of increased responsiveness to stimuli, has long been considered the underlying mechanism in insomnia, the precise etiology of insomnia has yet to be identified. Structural and functional neuroimaging are uncovering the physiological processes occurring in insomnia and have helped advance the general understanding of the pathophysiology of insomnia; this new information has the potential of offering greater insight into treatment and prevention.
In addition to the Stimulus Control Theory that hyperarousal processes play a key role in the development of insomnia, other conceptual models have been advanced which focus on the interaction between a variety of cognitive, neurocognitive and neurobiological mechanisms that may factor in the development of insomnia and prolong its duration.
Insomnia may occur alone or be associated with another sleep disorder, medical condition, psychiatric disorder, medication or substance use, or occur as a result of age-related changes in sleep requirements.
Insomnia has historically been classified according to chronicity, type or form, and subtype. Chronicity included transient, acute, and chronic. Type or form included primary and secondary insomnia – including, psychophysiological and comorbid insomnia, among other forms. Subtypes included early insomnia or sleep-onset insomnia, sleep maintenance insomnia or middle insomnia, terminal or late insomnia, or mixed insomnia- which is a combination of these three subtypes.
However, based on more recent research findings, the classification scheme in both the DSM and the ICSD has undergone significant change. In the most recent iterations of the DSM system, the concept of primary and secondary insomnia has been abolished, and in the ICSD system the detailed typing and subtyping of insomnia has been dropped. Despite these changes, many clinicians and researchers still use these terms:
- Primary insomnia is insomnia that cannot be attributed to a co-existing medical, psychiatric, or other health conditions.
- Secondary insomnia refers to insomnia either precipitated or associated with or co-occurring with another sleep disorder, medical or psychiatric disorder, drug or substance use.
- Psychophysiological insomnia is a subtype of the chronic insomnia disorder caused by an increased level of cognitive arousal, excessive worry about sleep, and learned maladaptive or sleep-preventing behaviors.
- Idiopathic insomnia is a lifelong inability to obtain adequate sleep with an onset during childhood that persists through adulthood.
- Paradoxical insomnia involves a discrepancy between subjective complaints of poor sleep and lab-based polysomnography findings.
- Substance-induced sleep disorder (insomnia type) results from the use of prescription, non-prescription, or illicit drugs and other substances such as food, alcohol, caffeine, tobacco, or withdrawal from hypnotic or anxiolytic drugs.
Both the DSM–5 and the ICSD-3 classification systems continue to differentiate insomnia based on chronicity (duration) as “episodic” or “short-term” if symptoms are present for a period lasting less than 3 months or occurring less than 3 or more times a week, and “persistent” or “chronic” if insomnia symptoms occur at least 3 times per week and last for 3 or more months. The DSM–5 replaced the term primary insomnia with insomnia disorder, and the ICSD-3 has simplified the categories to three: short-term insomnia disorder, chronic insomnia disorder, and other insomnia disorders.
Treatment Approaches
Many treatments are available for insomnia symptoms, including: sleep hygiene education, behavioral and psychological interventions, prescription and over-the-counter medications, and complementary and alternative medicine (CAM) treatments. The selection of the most appropriate treatment is dependent on the chronicity of symptoms, underlying medical/psychiatric factors and associated “3P factors” (predisposing, precipitating, and perpetuating).
Short-term insomnia can usually be treated by resolution or removal of the precipitating factor(s), good sleep habits, or short-term use of over-the-counter sleep remedies but may not require treatment at all. On the other hand, persistent or chronic insomnia requires early intervention and adequate treatment.
The two main types of clinical treatment for chronic insomnia, each having their own advantages and disadvantages, have been approved by the US Food and Drug Administration (FDA) are non-pharmacological treatment and pharmacological therapy.
- Non-pharmacological treatment includes psychological and behavioral treatments such as cognitive behavioral therapy (CBT-I), stimulus control therapy, relaxation training, sleep restriction therapy, or Multicomponent Behavioral Treatment for Insomnia.
- Pharmacological therapy includes several prescription drugs for insomnia. These include: nonbenzodiazepine hypnotics (zolpidem, eszopiclone), benzodiazepines (triazolam, temazepam), an orexin receptor antagonist (suvorexant), a melatonin agonist (ramelteon), and an antidepressant (doxepin). Only short-term use of pharmacological therapy is recommended.
Cognitive behavioral therapy, which is a structured program aimed at changing sleep habits and perpetuating factors which worsen sleep problems, is recommended as first-line treatment for all adults with chronic insomnia disorder.
Let’s review:
1. Which statement is not true about insomnia:
- Depression causes insomnia
- Insomnia is the most common sleep disorder
- There is no definitive diagnostic test for insomnia
- Insomnia occurs in both genders but is more prevalent in females.
2. Which of the following statements describe symptoms of insomnia:
- Inability to return to sleep after nocturnal awakenings
- Trouble staying asleep
- Difficulty waking up
- Difficulties falling asleep
Thanks for watching, and happy studying!
