Toxicity Reversal Agents

Hi, and welcome to this video about toxicity reversal agents!
Any substance, whether it’s over-the-counter, an illicit street drug, alcohol, or an herbal remedy, can be toxic. Toxic refers to the capability of a substance to cause injury or death, and drug toxicity refers to the adverse health effect caused by a drug.
Toxic effects of drugs are usually dose related, dependent on the amount, the concentration used, or the frequency of use, and usually occur at doses that exceed the drugs’ therapeutic range. The therapeutic range is the dosage range, blood plasma, or serum concentration range expected to achieve desired therapeutic results with minimal toxicity to most patients. However, therapeutic effects and toxic effects can occur simultaneously. Any organ or tissue in the body can be affected by drug toxicity: the kidneys, liver, and central nervous system being particularly susceptible; and it can affect multiple body systems or even the entire system.
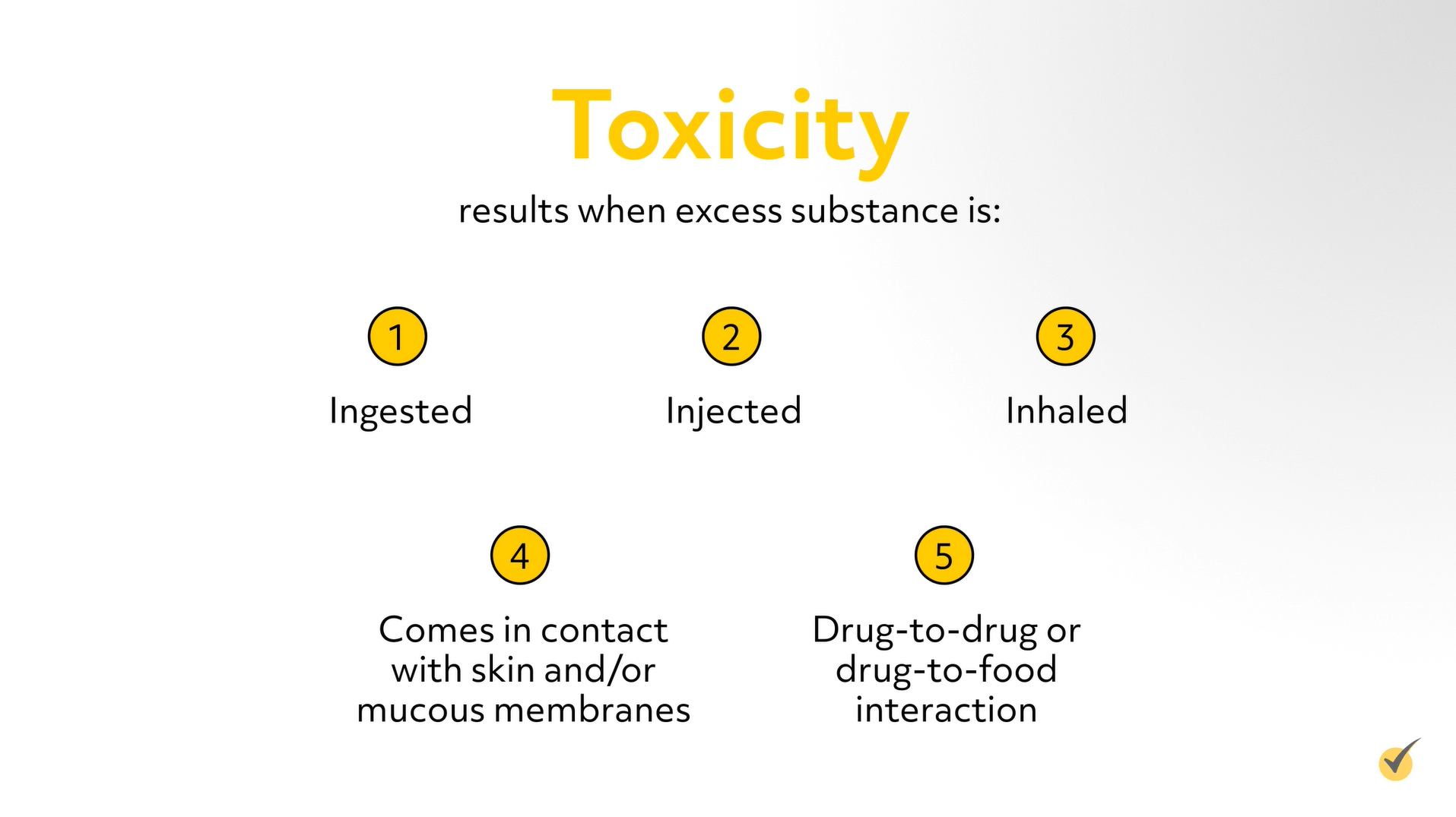
Commonly, toxicity results when excess substance is ingested, injected, inhaled, or comes in contact with skin and/or mucous membranes, but it may also occur as a result of a drug-to-drug or drug-to-food interaction. One should also note the physiological contributory factors of the person- such as age, body weight, pregnancy, genetics, and preexisting or concurrent diseases.
According to the National Poison Data System, the substances with the largest number of poisoning related deaths across all age groups include natural and synthetic opioids, sedatives and sleeping medications, stimulants, street drugs, and alcohol. This includes deaths resulting from unintentional and intentional overdoses, as well as taking the drug in error, inadvertently taking the drug, or being administered the wrong drug or drug dose.
Symptoms of toxicity vary depending on the substance (drug, chemical, or ingredient) involved, its physical and chemical properties, the amount, route, and its mechanism of action, and whether or not it was combined with another substance. Symptoms can include altered mental status, visual disturbances, nausea, vomiting, diarrhea, loss of motor coordination or balance, internal bleeding, cardiac irregularities, and respiratory depression.
When available, the appropriate and timely administration of a toxicity reversal agent can counteract the toxic action of the poison, enhance its elimination, and improve related morbidity and mortality. However, not every antidote is 100% effective and fatalities may still occur.
Toxicity Reversal Agents are available for a small number of drug toxicities, including alcohol induced toxicity, and are commonly referred to as an antidote. A toxicity reversal agent is defined as a drug that is used to reverse the effect of a narcotic, anesthetic, or potential toxic agent; while an antidote is simply defined as a substance that neutralizes or counteracts the effects of poison. Antidotes are classified according to the mode of action and can be a metabolic inhibitor, mechanical agent, chemical antagonist, competitive antagonist, non-competitive antagonist, chemical neutralizer, or oxidation-reduction agent. Some antidotes are very specific, working on only one type of poison, and others reverse the effects of many different types of poisons.
Common toxicity reversal agents include:
N-Acetylcysteine
N-Acetylcysteine (or Acetylcysteine, NAC) is used to treat acetaminophen (Tylenol) overdose, which is one of the most common poisonings.
Acetaminophen is a commonly used analgesic and antipyretic and is widely available in both prescription and OTC medications as a single ingredient or in combination medication products for colds, coughs, and pain relief. Acetaminophen is used in all age groups, including infants, toddlers, teenagers, and adults, and toxicity can result from either an acute overdose or from chronic overuse.
Initially, symptoms of acetaminophen poisoning, which are often mild and nonspecific, may not evolve for a number of hours. They include abdominal pain, nausea, vomiting, diarrhea, loss of appetite, and malaise. Progressively, symptoms of hepatic toxicity are most commonly jaundice, impaired coagulation, seizures, metabolic acidosis, and coma.
The antidote for acetaminophen poisoning, N-acetylcysteine (NAC), is available for both intravenous and oral administration. NAPQI is a toxic byproduct produced during the metabolism of acetaminophen; normally produced only in small amounts, and then immediately detoxified in the liver. NAC prevents the accumulation of NAPQI by increasing glutathione synthesis in the liver, preventing the binding of NAPQI to hepatic cells, reducing NAPQI back to acetaminophen and increasing sulfate conjugation, which enhances elimination of NAPQI.
Librium
Librium (chlordiazepoxide) is an anxiolytic drug, which is used to address specific symptoms that are associated with Alcohol Withdrawal Syndrome (AWS). AWS can occur when an individual, after a prolonged period of excessive alcohol use, either stops or significantly reduces their consumption. Individuals who “binge drink” (excessive alcohol use, either on a single occasion or as a regular practice) can also develop AWS.
Within hours after the last drink, the symptoms of AWS develop, peak within 72 hours, but may persist for a week or more. Symptoms can include:
- anxiety
- nausea
- abdominal pain
- cold sweats
- insomnia
Some develop life-threatening symptoms (Delirium tremens or DTs) which can include
- confusion
- agitation
- auditory and visual hallucinations
- dangerously high blood pressure
- a rapid pulse, a fever, and seizures.
- Left untreated, the DTs can cause respiratory or cardiovascular collapse and death
Gamma-aminobutyric acid
Gamma-aminobutyric acid (GABA) is the chief inhibitory neurotransmitter responsible for maintaining neurochemical balance in the brain. GABA reduces the effects of various excitatory neurotransmitters, like Glutamate, which is the primary excitatory neurotransmitter. During alcohol withdrawal, the levels of GABA decrease below normal. Without the inhibitory action of GABA, glutamate is activated, resulting in unregulated electrical excitation of the brain. Librium increases production of the GABA neurotransmitter, which decreases neuronal activity in the brain, reduces the psychomotor agitation, and prevents the progression from minor symptoms to life-threatening ones. Librium is available both orally and for intravenous administration, the dosage and route is dependent on the individuals’ vital signs, mental status, and degree of psychomotor agitation.
Flumazenil
Flumazenil (Romazicon) is the reversal agent of choice for an overdose of benzodiazepines, such as alprazolam, diazepam, or midazolam.
Benzodiazepines are a class of psychoactive drugs commonly known as minor tranquilizers. They enhance the effect of the neurotransmitter GABA, resulting in sedative, hypnotic, anticonvulsant, anxiolytic, and muscle relaxant properties. When an overdose of benzodiazepines is taken, it can cause extreme drowsiness, lack of coordination, slurred speech or confusion, difficulty breathing, and coma. Benzodiazepines are commonly abused and when taken in combination with other drugs of abuse, the potential for toxicity and fatality greatly increases.
Flumazenil is an antidote to counteract the toxic effects of benzodiazepines. It reverses the sedative effect, but is usually reserved for severe poisoning, because it can cause withdrawal and seizures in chronic benzodiazepine abusers. It has a short duration of action, so it may require repeated administrations with careful monitoring.
Lactulose
Lactulose (beta-galactosidofructose) is a non-absorbable disaccharide used to reduce blood ammonia levels in the treatment of Hepatic Encephalopathy (HE). Extremely toxic to the brain, an excessive accumulation of ammonia in the brain (ammonia toxicity) is responsible for the development of HE, which is also referred to as portosystemic encephalopathy (PSE).
Hepatic Encephalopathy can develop slowly over time and can be acute or chronic. This reversible condition has a spectrum of symptoms ranging from mild confusion and difficulty thinking to intracranial hypertension, loss of muscle control and coordination, impaired memory, seizures and coma; untreated severe HE can be fatal.
Lactulose, which is available as both a liquid and a powder, can be administered orally or rectally and decreases the concentration of ammonia in the blood by acidifying the contents of the colon. In the acidified environment, ammonia (NH3) is converted to ammonium ions (NH4+), inhibiting its diffusion from the colon into the blood, essentially trapping it in the colon. Reversely, the acidified environment enhances the diffusion of ammonia from the blood into the colon, decreasing the concentration of it in the blood. Furthermore, the cathartic action of Lactulose facilitates the elimination of the trapped ammonium ions from the colon.
Vitamin K (Phytonadione, Mephyton or AquaMephyton) is the reversal agent used to counter the effects of warfarin-based anticoagulants and warfarin-based rodenticides.
Warfarin
Warfarin, also known as coumadin, is the most commonly prescribed oral anticoagulant and can cause major or fatal bleeding. An overdose of warfarin can result from an inappropriately high dose, decrease in the intake of vitamin K, interaction of other drugs used simultaneously with warfarin, reduced synthesis or increased clearance of vitamin K-dependent clotting factors, alteration in protein binding interactions or ability, or an intentional overdose.
Reversing the effects of warfarin is recommended in the event of warfarin associated bleeding, or when the patient’s INR exceeds 4.5. Vitamin K can be administered either orally or by intravenous infusion, and unless rapid reversal of anticoagulation is necessary, the treatment of choice is oral vitamin K.
Digi bind
Digi bind (Digoxin Immune Fab, Digifab) is used to treat the presence of hyperkalemia or life-threatening dysrhythmias from digoxin and related cardiac glycosides toxicity.
Toxicity can emerge during long-term therapy with digoxin, or ingestion of naturally occurring compounds containing cardiac glycosides e.g., Foxglove (Digitalis), Lily of the Valley (Convallaria majalis), and Common Oleander (Nerium oleander), or after an accidental or intentional overdose. Symptoms of toxicity can also occur when serum digoxin concentration is within the therapeutic range due to some overlap between therapeutic and toxic serum digoxin levels.
Digi bind, which is administered by the intravenous route, binds molecules of digoxin, making them unavailable for binding at their usual sites of action in the body.
Protamine sulfate
Protamine sulfate is used to reverse the anticoagulant effects of unfractionated heparin and low-molecular weight heparin (enoxaparin, Lovenox, tinzaparin sodium (INNOHEP) and dalteparin (Fragmin)). Heparin, an indirect thrombin inhibitor, suppresses coagulation by binding with—and activating—antithrombin, which inactivates multiple factors in the coagulation cascade, principally thrombin and factor Xa.
Heparin
Heparin is used in a variety of different clinical situations. It is the most commonly used anticoagulant for short term therapy and the drug of choice for the initial treatment of a pulmonary embolism, deep venous thrombosis, transient ischemic attack (TIA), ischemic stroke and acute myocardial infarction. It is used in the prophylaxis and treatment of thrombo-embolic disorders, to prevent clotting during various surgical procedures, hemodialysis, and blood transfusions, and in treatment of acute and chronic coagulopathies (disseminated intravascular coagulation.)
Heparin is classified as a high-risk drug; an overdose can cause excessive bleeding and life-threatening blood loss. At higher doses, heparin interferes with platelet aggregation, prolongs bleeding time and an overdose impairs the body’s ability to form blood clots. The amount of heparin that is toxic is different for each individual, and the dosage of heparin should be adjusted according to the individual’s coagulation test results.
Protamine sulfate is indicated in the treatment of a heparin overdose, hemorrhages associated with its use; and to reverse its effects during neuro, cardiothoracic and vascular surgery, obstetrical deliveries, blood transfusions or dialysis procedures. Protamine sulfate is administered intravenously and forms a strong bond with the heparin, producing a stable salt complex that has no anticoagulant activity.
Deferoxamine
Deferoxamine (Desferal, DFO) is an iron-chelating agent and is used in the treatment of acute iron poisoning (toxicity) and iron overload. Iron is an essential micronutrient required for a variety of biochemical processes in the body, including the transport and storage of oxygen, the formation of iron-containing enzymes and cellular growth and proliferation.
While eating a well-balanced diet can provide an individual with enough iron to meet requirements, iron is a common dietary deficiency worldwide. Acute or chronic blood loss, an alteration in iron absorption, medications or food sources that inhibits iron absorption; and several conditions or diseases such as celiac disease, Crohn’s disease, and gastric bypass surgery, can also cause an iron deficiency. Iron supplements are used in the treatment of this deficiency, typically as multivitamins with iron, ferrous sulphate, or ferrous gluconate tablets. These supplements are widely used and are available both with and without a prescription.
Iron, a heavy metal, is toxic to the central nervous system, GI, and cardiovascular system, with iron toxicity being a leading cause of poisoning deaths in children. While rare in adults, iron overdose occurs when someone of any age, accidentally or intentionally, takes more than the normal or recommended amount of iron.
Symptoms of iron toxicity include nausea, vomiting, diarrhea, fever, and abdominal pain and can rapidly progress to lethargy, metabolic acidosis, seizures, multisystem failure, and even death.
Deferoxamine is used for the treatment of iron toxicity. Patients with severe gastroenteritis, those with serum iron level > 500 μg/dL) as well as those in metabolic acidosis or shock are treated with deferoxamine to chelate ferric (Fe3+) iron.
Deferoxamine, which is available for intramuscular, subcutaneous, and intravenous administration, binds with ferric (Fe3+) iron to form ferrioxamine, which is eliminated via the kidneys, reducing the excess of unbound iron.
Naloxone
Naloxone (Narcan, Evzio) is used for the reversal of the serious and potentially life‐threatening complication of opioid overdose, abuse, or misuse (respiratory depression).
Opioids, a broad class of drugs, are either naturally derived from opium (opiates) or synthetically manufactured, and include but are not limited to, codeine, morphine, oxycodone, hydrocodone, fentanyl, hydromorphone, oxymorphone, methadone, and the illegal drug heroin. Opioids are the most commonly used drug to treat moderate to severe acute and chronic pain.
Opioids bind to and activate opioid receptors located both in the central nervous system and throughout the body, blocking pain signals sent from the brain to the body and producing a system wide effect that includes, feelings of euphoria, sedation, decreased gastrointestinal (GI) motility, miosis, hypotension, and irregular, shallow and decreased respiratory rate.
Naloxone, an opioid receptor antagonist, binds to opiate receptors and acts as a competitive inhibitor to both natural and synthetic opioids, rapidly reversing all the pharmacological effects, including respiratory depression, sedation, and hypotension.
Naloxone can be administered nasally, subcutaneously, intramuscularly, intravenously, or intraosseously. While effective when administered orally, a much larger dose would be required, therefore it is seldom used.
Let’s Review with a couple of questions:
1. Which statement is not true about toxic reversal agents?
- Toxic reversal agents are drugs that are used to reverse the effect of a narcotic, anesthetic, or potential toxic agent.
- Toxic reversal agents are available for all prescriptions and over the counter medications.
- Toxic reversal agents neutralize or counteract the effects of another drug through a variety of mechanisms, and can be classified based on their mode of action.
- Toxic reversal agents are not 100% effective.
If you chose B, you are correct! Toxicity reversal agents are available for a small number of drugs, including alcohol.
2. Which statements are true about the toxic effects of drugs?
- The toxic effect of a drug will always cause permanent damage.
- Symptoms of drug toxicity vary depending on the substance, the amount ingested, and whether or not it was combined with another substance.
- Toxic effects of drugs are usually dose related, and usually happen at doses that exceed the drugs’ therapeutic range
- Most exposures to toxic drugs occur in the home setting, are unintentional, involve children under the age of 6, involve one substance, and result in fatal toxic reactions.
- The vast majority of poisoning deaths are attributed to drugs—illegal, prescription, or over-the-counter drugs.
If you chose B, C, and E, you are correct.
Thanks for watching, and happy studying!