
Welcome to this video on assessment tools for pain
Assessment tools for pain are instruments that help you measure a patient’s degree of pain in addition to assessing patients’ conditions and needs. Some assessment tools for pain are observational, based on patients’ responses that can be seen, such as their expressions and body positions.
Other tools are subjective and based on the patients’ own self-assessments of their pain, usually guided by some type of scale.
In this video, you will learn about some of the most common assessment tools for pain, including:
- The Wong-Baker Faces Pain Scale
- The numeric pain rating scale
- The visual analog scale
- Categorical scales
- The brief pain inventory
- The McGill Pain Questionnaire
- The critical care pain observation tool (CPOT)
Wong-Baker Faces Pain Scale
First, let’s look at the Wong-Baker Faces Pain Scale. This scale was originally designed for children ages 3 and older and is most commonly used for preschoolers and young children who are not yet able to use numbers to rate their level of pain. Children choose a face that matches their level of pain.
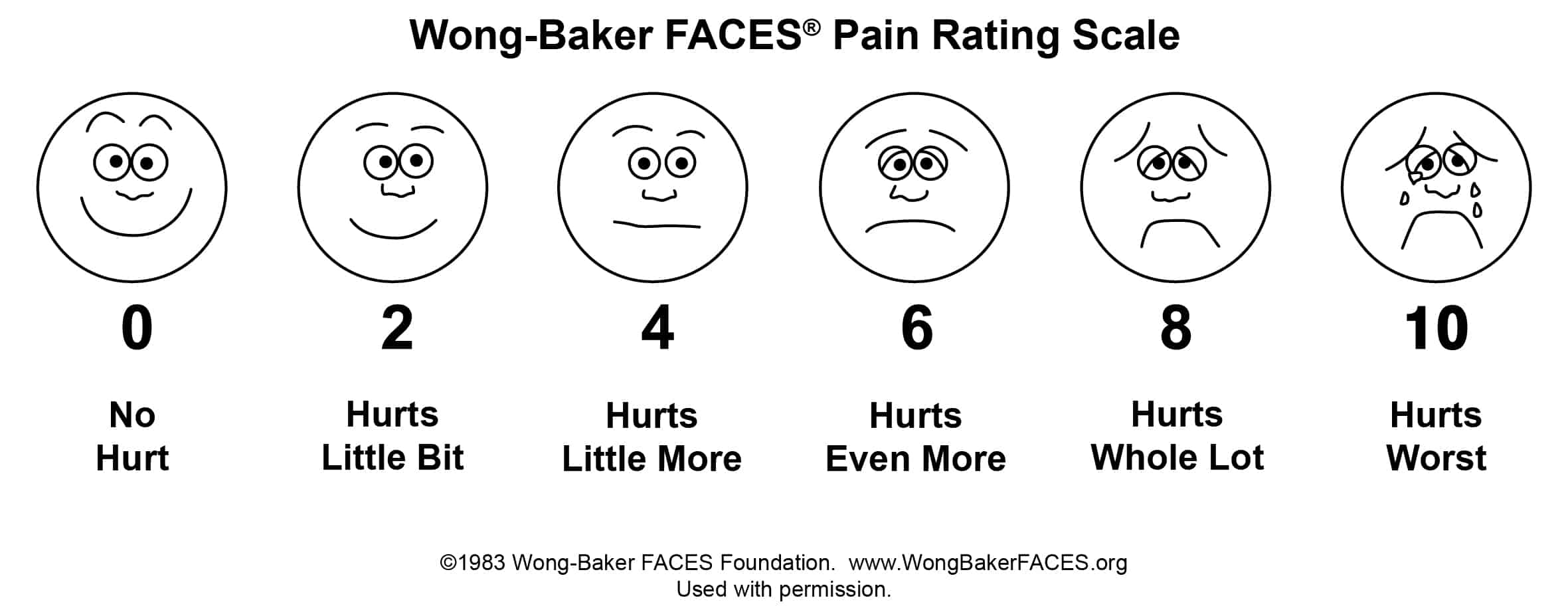
The Wong-Baker Faces Pain Scale can also be used with adults, especially those with language barriers or intellectual disabilities.
Numeric Pain Rating Scale
Next, the numeric pain rating scale is the scale most commonly used for children 6 years and older, adolescents, and adults. Patients are instructed with a statement such as, “On a scale of 0 to 10 with 0 being no pain and 10 being the worst pain you can imagine, how do you rate your pain?”
With the numeric pain rating scale, the score represents the degree of pain:
- 0 represents no pain
- 1 to 3 represents mild pain
- 4 to 6 represents moderate pain AND
- 7 to 10 represents severe pain
Visual Analog Scale
The visual analog scale is similar to the numeric pain rating scale but usually lacks the intervening numbers between 0 and 10. The visual analog scale indicates the intensity of pain only.
Patients are instructed, “If the beginning of the line is no pain and the end of the line is the worst pain you can imagine, where on the line is your pain?” Patients then place a mark or point to a spot on the line that represents their degree of pain.
Categorical Scales
In addition to the other types of scale, categorical scales depend on words rather than numbers to indicate the intensity of pain. Categorical scales are appropriate for children 7 and older with adequate reading and comprehension skills and adults with adequate mental abilities and language skills.
One example of a categorical scale is the verbal pain intensity scale, which rates the intensity of pain as no pain, mild pain, moderate pain, severe pain, very severe pain, and worst possible pain.
Brief Pain Inventory (BPI)
Another pain assessment tool that is more comprehensive is the brief pain inventory (BPI). The brief pain inventory is intended primarily for adults but may be used with some adolescents, such as those with rheumatoid arthritis. The brief pain inventory is used to assess clinical pain, such as cancer pain or other chronic pain. The brief pain inventory includes body illustrations so that the patient can indicate locations of pain.
The brief pain inventory also includes a number of numeric scales (1-10) that assess different aspects of pain. These include:
- Worst pain in previous 24 hours
- Least pain in previous 24 hours
- Average pain
- Current pain
- Pain relief in percentage from medications in the previous 24 hours
- Pain interference in the previous 24 hours with general activity, mood, walking ability, normal work ability (outside and housework), relations with other people, sleep, and enjoyment of life
McGill Pain Questionnaire
Next, the McGill Pain Questionnaire is a self-reporting tool intended for adult patients with significant pain from cancer or other types of chronic pain. This tool helps to assess changes over time and response to interventions. Both a short version and a long version are available. The long version contains 20 different dimensions of pain (such as temporal, spatial, and constrictive pressure).
Each dimension has 1 to 5 descriptors that are assigned points. The patient chooses the most appropriate descriptor for each dimension. For example:
- Pinching: 1 point
- Pressing: 2 points
- Gnawing: 3 points
- Cramping: 4 points
- Crushing: 5 points
In addition, the McGill Pain Questionnaire asks the patient to choose descriptors about:
- How pain changes over time: patterns of pain, items that increase or decrease pain
- Strength of pain: current pain, worst pain, least pain
The higher the total score, the greater the pain.
Critical Care Pain Observation Tool (CPOT)
Last, the critical care pain observation tool (CPOT) is an observational tool for a specific population of adults that are in critical care and who are:
- Unable to self-report
- Intubated
- Sedated
The critical care pain observation tool assesses pain on a 0 to 2 scale by observation of:
- Facial expression
- Body movements
- Muscle tension
- Compliance with ventilator, if intubated
- Vocalization, if extubated
A score of equal to or greater than 2 indicates pain.
Choosing an appropriate pain assessment tool and carrying out routine assessment is critical to pain management, but it’s important to remember that the pain assessment tool should be a first step in pain assessment, not the only step. Many of these pain assessment tools, such as the numeric pain rating scale, consider only the intensity of pain.
However, pain is multidimensional, and pain assessment should be, likewise, multidimensional, considering such factors as duration, location, emotional response, physical response, aggravating factors, and mitigating factors.
Thanks for watching, and happy studying!
